Tim Pittman
Articles by Tim Pittman

Cardiology & Heart Surgery
The incidence of heart failure (HF) continues to increase rapidly—exceeding six million patients in the U.S., according to the CDC—but new clinical developments may trigger a much more significant hike in HF within the next decade.
The lingering effects of long-COVID and long-term consequences of nonalcoholic fatty liver disease (NAFLD) are the primary drivers, says Marat Fudim, MD, MHS, a Duke advanced heart failure specialist and director of remote cardiac monitoring.
While the two HF subtypes are estimated to be equal in prevalence, Fudim says, the diagnosis of HF with preserved ejection fraction (HFpEF) is more challenging than HF with reduced ejection fraction (HFrEF).
The major challenge in diagnosing HFpEF is the constellation of diverse symptoms that may be present among patients. Shortness of breath is a common reason patients seek care, but it is often associated with comorbidities.
“Because of our aging population and obesity crisis, we see an enormous heart failure wave forming and it’s rolling our way,” Fudim says. “This will present significant risk to our health care systems because of the thousands of hospitalizations these patients will require.”
Fudim estimates that HF incidence within the U.S. may be higher than the CDC projects because a large portion of patients with HFpEF are either undiagnosed or misdiagnosed with other conditions. “The combination of these factors will force a paradigm shift in our approach to and management of the HF in the future,” he says.
Analyzing national COVID hospitalization rates, Fudim and colleagues estimate that 46% of patients hospitalized with long COVID developed HF symptoms within 12 months. The CDC reports that approximately 7.5% of the US population has long COVID symptoms, defined as lasting three or more months since first contracting the virus. Even if patients with COVID are not hospitalized, they continue to be at risk of developing long COVID, which mimics HF symptoms.
The lingering effects of long-COVID and long-term consequences of nonalcoholic fatty liver disease (NAFLD) are the primary drivers, says Marat Fudim, MD, MHS, a Duke advanced heart failure specialist and director of remote cardiac monitoring.
While the two HF subtypes are estimated to be equal in prevalence, Fudim says, the diagnosis of HF with preserved ejection fraction (HFpEF) is more challenging than HF with reduced ejection fraction (HFrEF).
The major challenge in diagnosing HFpEF is the constellation of diverse symptoms that may be present among patients. Shortness of breath is a common reason patients seek care, but it is often associated with comorbidities.
“Because of our aging population and obesity crisis, we see an enormous heart failure wave forming and it’s rolling our way,” Fudim says. “This will present significant risk to our health care systems because of the thousands of hospitalizations these patients will require.”
Fudim estimates that HF incidence within the U.S. may be higher than the CDC projects because a large portion of patients with HFpEF are either undiagnosed or misdiagnosed with other conditions. “The combination of these factors will force a paradigm shift in our approach to and management of the HF in the future,” he says.
Analyzing national COVID hospitalization rates, Fudim and colleagues estimate that 46% of patients hospitalized with long COVID developed HF symptoms within 12 months. The CDC reports that approximately 7.5% of the US population has long COVID symptoms, defined as lasting three or more months since first contracting the virus. Even if patients with COVID are not hospitalized, they continue to be at risk of developing long COVID, which mimics HF symptoms.

Interdisciplinary
Two surgeons are collaborating to offer peripheral nerve care by combining surgical repair with nerve restoration therapy in one of the first practices of its kind in the Carolinas. Brandon W. Smith, MD, a neurosurgeon, Neill Y. Li, MD, an orthopaedic surgeon, work together to treat patients with peripheral nerve injuries related to trauma, stroke or spinal cord injuries that affect upper motor neurons.
Peripheral nerve clinic care has improved significantly in the past decade as a result of research-based regeneration therapies, the surgeons say. Specialists can repair and reconstruct upper motor neuron injuries in the brain or spinal cord and offer improved outcomes that may restore limb movement or sensation.
Smith specializes in peripheral nerve and spinal procedures including neve entrapment and tumors, ganglion cysts, and brachial plexus injuries. Li focuses on surgery of the hand and upper extremities and has advanced training in microvascular surgery.
“We are already providing these therapies to patients, but we have a vision for a single-visit clinic at which a patient can see a neurologist, a pain specialist, a neurosurgeon, and an orthopaedic surgeon at the same location,” says Smith. “Many of these patients have difficulty coming to multiple visits with specialists. We want to create a coordinated care center to address this need.”
Patients benefit now from their existing multidisciplinary collaboration, but both surgeons promote the efficiency and convenience of a one-stop clinic offering a holistic focus on the patient’s overall health.
Peripheral nerve clinic care has improved significantly in the past decade as a result of research-based regeneration therapies, the surgeons say. Specialists can repair and reconstruct upper motor neuron injuries in the brain or spinal cord and offer improved outcomes that may restore limb movement or sensation.
Smith specializes in peripheral nerve and spinal procedures including neve entrapment and tumors, ganglion cysts, and brachial plexus injuries. Li focuses on surgery of the hand and upper extremities and has advanced training in microvascular surgery.
“We are already providing these therapies to patients, but we have a vision for a single-visit clinic at which a patient can see a neurologist, a pain specialist, a neurosurgeon, and an orthopaedic surgeon at the same location,” says Smith. “Many of these patients have difficulty coming to multiple visits with specialists. We want to create a coordinated care center to address this need.”
Patients benefit now from their existing multidisciplinary collaboration, but both surgeons promote the efficiency and convenience of a one-stop clinic offering a holistic focus on the patient’s overall health.

Transplant
The Duke Lung Transplant program is expanding patient outreach and by securing state licenses that allow transplant pulmonologists to use telehealth to communicate with patients outside North Carolina. The use of telehealth soared during the COVID-19 pandemic and, as a result, many states waived restrictions governing telehealth communications with out-of-state patients to reduce the risks of travel.
Interdisciplinary
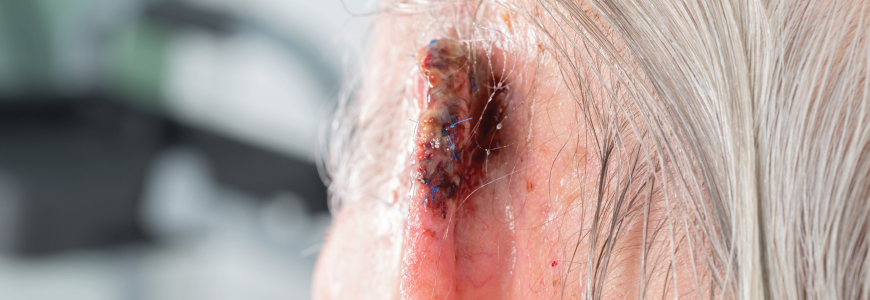
mproving melanoma treatment among older patients is a key focus for Jay S. Lee, MD, a Duke surgical oncologist working to uncover age-specific outcome data while engaging patients to better understand their treatment goals.
Lee, who sees patients at Duke Raleigh in Wake County and at Duke Hospital in Durham, is one of several Duke Health physicians offering clinical trials for new melanoma therapies.
Immunotherapy has dramatically improved the effectiveness of treatments for patients with more advanced melanoma, Lee says. These treatments can reduce the need for surgery in some cases and help oncologists reduce or halt the spread of melanoma. Early diagnosis remains a key to improved outcomes.
But the effects of immunotherapy are less well known for patients in their late 70s and beyond, Lee cautions. The lack of data hampers treatment strategies for senior patients.
“The evidence is simply not as clear for older patients,” Lee says. “We need more evidence to help us understand how older patients respond to immunotherapy.“Another factor in planning treatment is that we often have a poor and incomplete understanding of what older patients want regarding outcomes following their treatment for melanoma,” Lee says. “Many older patients may be concerned about how cancer treatment will affect their quality of life.”
Lee, who sees patients at Duke Raleigh in Wake County and at Duke Hospital in Durham, is one of several Duke Health physicians offering clinical trials for new melanoma therapies.
Immunotherapy has dramatically improved the effectiveness of treatments for patients with more advanced melanoma, Lee says. These treatments can reduce the need for surgery in some cases and help oncologists reduce or halt the spread of melanoma. Early diagnosis remains a key to improved outcomes.
But the effects of immunotherapy are less well known for patients in their late 70s and beyond, Lee cautions. The lack of data hampers treatment strategies for senior patients.
“The evidence is simply not as clear for older patients,” Lee says. “We need more evidence to help us understand how older patients respond to immunotherapy.“Another factor in planning treatment is that we often have a poor and incomplete understanding of what older patients want regarding outcomes following their treatment for melanoma,” Lee says. “Many older patients may be concerned about how cancer treatment will affect their quality of life.”

Interdisciplinary
For more than two years, Duke Health has been building a comprehensive Fontan program designed for patients with single-ventricle heart disease by bringing together a team of experts across multiple organ systems for surveillance and monitoring.
Patients with single ventricle heart disease require multiple surgeries during early childhood that culminate in what is described as Fontan physiology or circulation. The Duke Fontan program is customized to help manage the complications these patients experience as they grow.

Transplant
Simultaneous pancreas and kidney transplant (SPK) has yielded promising outcomes for patients with challenging Type 2 Diabetes Mellitus (T2MD) and may prove particularly important to patients dealing with health care disparities who have limited access to diabetes therapies.
Lisa McElroy, MD, MS, a Duke abdominal transplant surgeon and researcher, encourages more frequent consideration of SPK as an option for many patients with T2DM and kidney damage.
“Some specialists suggest that pancreas transplant has been rendered extinct because of the availability of insulin pumps and monitors for patients with diabetes,” McElroy says. “But this is actually a falsehood because a substantial number of patients with diabetes simply lack access to these advanced therapies.”
Lisa McElroy, MD, MS, a Duke abdominal transplant surgeon and researcher, encourages more frequent consideration of SPK as an option for many patients with T2DM and kidney damage.
“Some specialists suggest that pancreas transplant has been rendered extinct because of the availability of insulin pumps and monitors for patients with diabetes,” McElroy says. “But this is actually a falsehood because a substantial number of patients with diabetes simply lack access to these advanced therapies.”
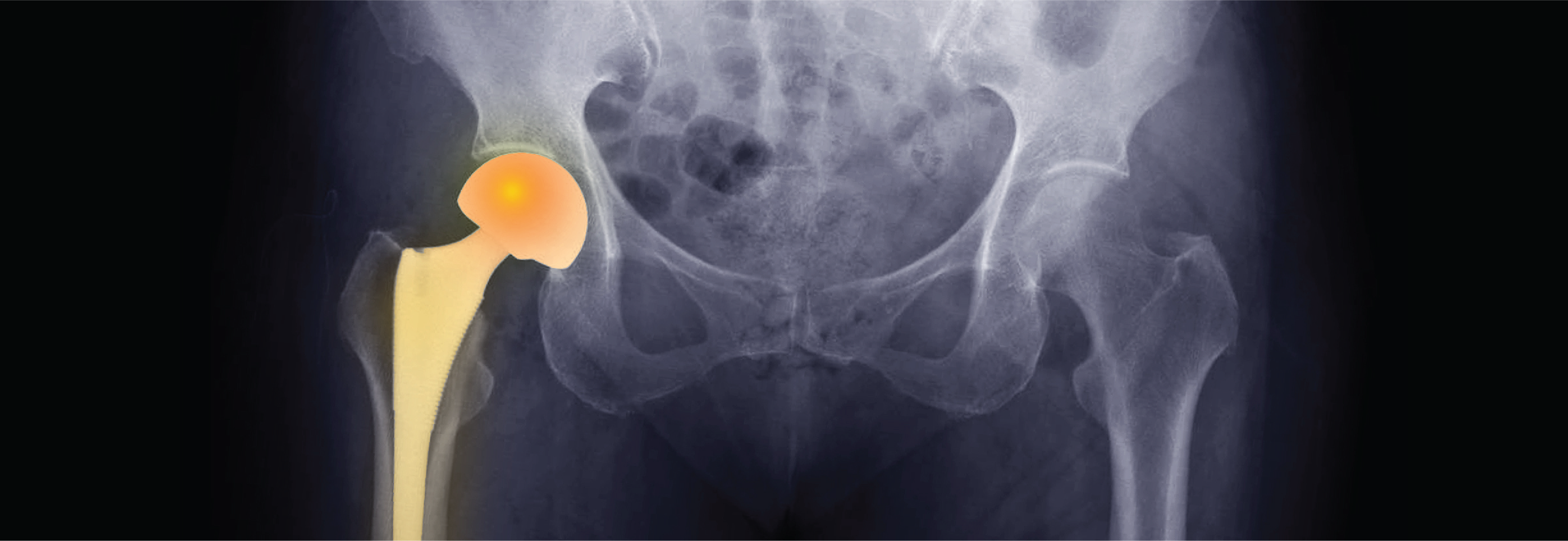
Orthopaedics
Duke orthopaedic surgeons continue to advance the still-novel use of augmented reality (AR) to assist in hip replacement during complex procedures to improve accuracy and outcomes. Sean P. Ryan, MD, an orthopaedic surgeon in the Duke Division of Adult Reconstruction, works with Samuel S. Wellman, MD, in one of the nation’s first AR-assisted hip replacement programs.
“Because of our commitment to minimize complications, we are always looking for ways to deliver better patient outcomes,” Ryan says. “This is the most effective innovation we’ve worked with and it’s showing tremendous promise.”
The AR-guided platform has the potential to increase surgical efficiency and accuracy in total hip arthroplasty (THA). The technology allows surgeons to view 3D models of the patient’s anatomy, implants, and instruments inside the body in real time intraoperatively.
“Our primary focus is securing an accurate placement, which minimizes the risk of a dislocation,” Ryan says. “Unfortunately, as all surgeons know, dislocation remains a significant problem.” The technology is particularly valuable for patients with complex presentations who are at risk of dislocation, Ryan adds.
Patients with arthritis or complex pathologies who need a hip replacement receive a CT scan before surgery. When perioperative preparations are completed, surgeons attach an overlay to the pelvis before donning goggles that provide an AR-enhanced view. An illuminated arrow appears in the goggle screen to guide the procedure.
“Because of our commitment to minimize complications, we are always looking for ways to deliver better patient outcomes,” Ryan says. “This is the most effective innovation we’ve worked with and it’s showing tremendous promise.”
The AR-guided platform has the potential to increase surgical efficiency and accuracy in total hip arthroplasty (THA). The technology allows surgeons to view 3D models of the patient’s anatomy, implants, and instruments inside the body in real time intraoperatively.
“Our primary focus is securing an accurate placement, which minimizes the risk of a dislocation,” Ryan says. “Unfortunately, as all surgeons know, dislocation remains a significant problem.” The technology is particularly valuable for patients with complex presentations who are at risk of dislocation, Ryan adds.
Patients with arthritis or complex pathologies who need a hip replacement receive a CT scan before surgery. When perioperative preparations are completed, surgeons attach an overlay to the pelvis before donning goggles that provide an AR-enhanced view. An illuminated arrow appears in the goggle screen to guide the procedure.

Oncology
By focusing on relationships with referring physicians and offering comprehensive, convenient care for patients, leaders of the Duke Raleigh Cancer Center’s Genitourinary (GU) Clinic say they are working to establish a new care model for prostate cancer in Wake County. Sundar Ramalingam, MD, a hematologist and medical oncologist, focuses primarily on patients with prostate cancer and other urologic malignancies. Duke’s team-based approach to prostate cancer offers many advantages for patients and referring providers, he says.
“As an academic medical center, we have access to the latest research and we offer patients opportunities to participate in clinical trials,” Ramalingam says. “Our patients also benefit from clinical assessments by our tumor board, which considers each situation individually as well as consultations with experts in every dimension of care for patients with prostate cancer.”
New treatments are being discovered regularly for diseases such as prostate cancer, Ramalingam says. “We are able to offer early access to some treatments. These potential therapies offer promise for future treatments.” Ramalingam and colleagues also emphasize prompt access to GU clinic care following a cancer diagnosis. “We want patients to begin their care as soon as possible,” he says. “Access to prompt care is a significant factor in managing this condition.”
The GU team emphasizes patient convenience, Ramalingam says. Patient visits are scheduled to take advantage of special clinics in which both medical and surgical specialists are available to discuss treatment plans. In addition to the physicians, the clinic’s care team takes a proactive approach to simplify the patient experience, Ramalingam adds.
“As an academic medical center, we have access to the latest research and we offer patients opportunities to participate in clinical trials,” Ramalingam says. “Our patients also benefit from clinical assessments by our tumor board, which considers each situation individually as well as consultations with experts in every dimension of care for patients with prostate cancer.”
New treatments are being discovered regularly for diseases such as prostate cancer, Ramalingam says. “We are able to offer early access to some treatments. These potential therapies offer promise for future treatments.” Ramalingam and colleagues also emphasize prompt access to GU clinic care following a cancer diagnosis. “We want patients to begin their care as soon as possible,” he says. “Access to prompt care is a significant factor in managing this condition.”
The GU team emphasizes patient convenience, Ramalingam says. Patient visits are scheduled to take advantage of special clinics in which both medical and surgical specialists are available to discuss treatment plans. In addition to the physicians, the clinic’s care team takes a proactive approach to simplify the patient experience, Ramalingam adds.

Cardiology & Heart Surgery
The Duke Adult Congenital Heart Center is expanding therapeutic options for patients with congenital heart disease (CHD) as clinical leaders prepare to manage a surge in patients.
Working closely with the Pediatric Congenital Heart Team and several other subspecialties, leaders of the adult congenital program have analyzed and adopted new methods to help patients transition from pediatric to adult CHD care while launching new clinics to incorporate novel therapeutic approaches.
The number of adults with CHD in the U.S. grows by approximately 40,000 patients annually, says Richard A. Krasuski, MD, director of the Duke Adult Congenital Heart Center, and now totals more than two million.
“Our collaboration with the Duke Pediatric Team has helped to identify higher risk populations that require more specialized care,” Krasuski says. “This group includes patients born with single ventricles palliated with Fontan surgery. Many of these patients develop problems that involve many organ systems, sometimes even requiring organ transplantation.
“We have developed clinics for Fontan management and heart failure/transplantation assessment and management,” he adds. “It’s a very complex population that is steadily growing.”
The pediatric-adult partnership also creates a seamless clinical transition for patients who require adult care. “This transition is critical period in the life of a young adult,” Krasuski says. “Our team-based approach helps patients make the transition safely and smoothly.”
Patient care extends throughout the lifespan, and Duke’s record of novel clinical interventions—new medications, stents or pioneering surgical procedures—has helped the center serve older patients with CHD more effectively.
Working closely with the Pediatric Congenital Heart Team and several other subspecialties, leaders of the adult congenital program have analyzed and adopted new methods to help patients transition from pediatric to adult CHD care while launching new clinics to incorporate novel therapeutic approaches.
The number of adults with CHD in the U.S. grows by approximately 40,000 patients annually, says Richard A. Krasuski, MD, director of the Duke Adult Congenital Heart Center, and now totals more than two million.
“Our collaboration with the Duke Pediatric Team has helped to identify higher risk populations that require more specialized care,” Krasuski says. “This group includes patients born with single ventricles palliated with Fontan surgery. Many of these patients develop problems that involve many organ systems, sometimes even requiring organ transplantation.
“We have developed clinics for Fontan management and heart failure/transplantation assessment and management,” he adds. “It’s a very complex population that is steadily growing.”
The pediatric-adult partnership also creates a seamless clinical transition for patients who require adult care. “This transition is critical period in the life of a young adult,” Krasuski says. “Our team-based approach helps patients make the transition safely and smoothly.”
Patient care extends throughout the lifespan, and Duke’s record of novel clinical interventions—new medications, stents or pioneering surgical procedures—has helped the center serve older patients with CHD more effectively.
Transplant
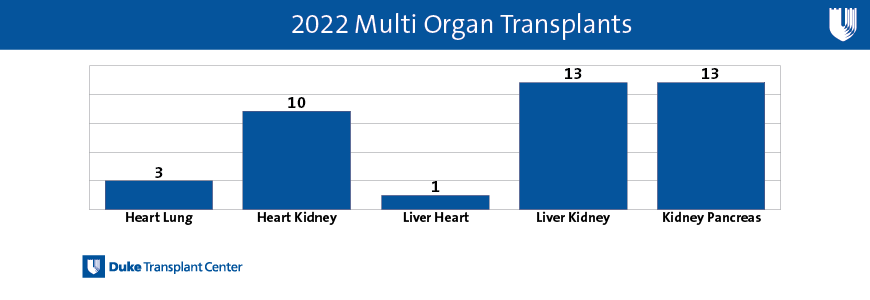
Duke transplant specialists performed 40 multi-organ procedures during 2022, an accomplishment that places the program in the top ten nationally, according to data from the Organ Procurement and Transplantation Network (OPTN).
The high ranking among major medical centers highlights the success of a cohesive, high-performance program, says Ian R. Jamieson, MBA, MHA, vice president of the Duke Transplant Center. Significantly, outcomes for patients undergoing those procedures are also excellent, he adds. The 2022 data indicates an increase over the team’s 38 multi-organ transplants during 2021.
“Whenever a medical center completes a multi-organ transplant, it’s evidence that your team is working at the top of its game,” Jamieson says. “We are proud to have highly functioning teams across all organ programs functioning with a high level of multi-disciplinary cooperation.”
The high ranking among major medical centers highlights the success of a cohesive, high-performance program, says Ian R. Jamieson, MBA, MHA, vice president of the Duke Transplant Center. Significantly, outcomes for patients undergoing those procedures are also excellent, he adds. The 2022 data indicates an increase over the team’s 38 multi-organ transplants during 2021.
“Whenever a medical center completes a multi-organ transplant, it’s evidence that your team is working at the top of its game,” Jamieson says. “We are proud to have highly functioning teams across all organ programs functioning with a high level of multi-disciplinary cooperation.”

