A rapidly growing multidisciplinary program developed by Duke’s divisions of Thoracic Surgery and Gastroenterology is offering a new level of care for patients with GERD, esophageal dysphagia, achalasia, and other esophageal motility disorders. Through this distinctive program, specialists are coordinating and improving access to care, offering the most advanced diagnostic and therapeutic techniques, developing patient-centered programs and support groups, and initiating research to help address complex conditions.
“For selected patients with the most complex needs, we can deliver real-time evaluation by both gastroenterologists and surgeons in our clinic,” says gastroenterologist Rahul A. Shimpi, MD.
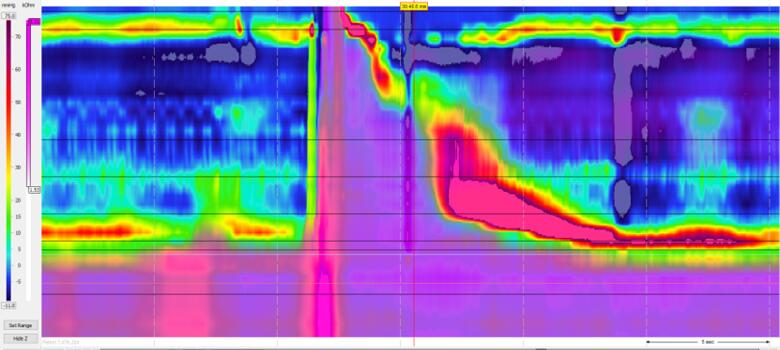
These patients typically require advanced diagnostic testing and therapeutic care, so they often need to be seen in multiple settings for endoscopy, esophageal manometry, reflux testing, barium swallows, CTs, and surgery. Shimpi says the esophageal center aims to make the referral and scheduling process more efficient by minimizing the number of visits patients need to make. “These patients often need multidisciplinary care for the best outcomes. Here at Duke, it’s about how we can evaluate these patients together and come up with the best course of management.”
Duke’s esophageal patient referral volume has increased dramatically over the past three years, with much of the increase due to an expanding array of diagnostic techniques and surgical and nonsurgical options, Shimpi reports. “Five years ago, if a patient had GERD, their options for management were either anti-reflux medications or laparoscopic Nissen fundoplication. Now we can offer other, less invasive surgical or endoscopic options, including the LINX device (Torax Medical Inc., Shoreview, MN), transoral incisionless fundoplication (TIF, EndoGastric Solutions, Inc., Redmond, WA), Stretta Therapy (Restech, Houston, TX), and there is a new class of promising medications currently in clinical trials.”
Many opportunities exist for patients facing a variety of esophageal disorders to receive the latest treatment options through clinical trials and registries. David A. Leiman, MD, MSHP, is the Director of Esophageal Research and Quality for the Gastroenterology division at Duke and the Principal Investigator for several ongoing and upcoming clinical trials in the center, including the study of novel therapeutics for patients with GERD, erosive esophagitis, and eosinophilic esophagitis (EoE).
Among the center’s other planned research initiatives are leveraging the extensive expertise in pulmonary and esophageal diseases to better understand the unique interplay between these entities and defining testing protocols for their evaluation. For example, Matthew G. Hartwig, MD, a thoracic surgeon and the surgical director for the Esophageal Center at Duke, is leading a registry to evaluate using the newest interventions for reflux to protect newly transplanted lungs from ongoing injury. Because “there’s no set algorithm for this type of testing or treatment, everyone does it a little differently across the country, and it’s not data-driven. It makes a lot of sense to collect the patient data and turn it into a robust research program,” says Shimpi.
Building on their clinical experience and insights from prior studies, Leiman says “the goal is to create the definitive evidence-based protocol.” Future work will also aim to transform the data from routine clinical interactions into a comprehensive esophageal diseases registry to evaluate and improve patient outcomes.
Shimpi notes that many patients seek second, third, or even fourth opinions from Duke specialists and surgeons. “Often times they’ve had esophageal surgery or a procedure elsewhere and either their condition didn’t improve, or they have a new iatrogenic esophageal problem as a result. We are very proud to offer the most advanced diagnostics and therapeutics; when it comes to benign esophageal disease, we do it all at a very high level,” he says.
“Duke’s success at centralizing and coordinating experts in diseases of the foregut throughout the multidisciplinary spectrum culminates from years of work by individuals across the health system. It’s exciting to see this taking shape for the first time at Duke and even more rewarding to see it pay off in terms of better, more efficient care for our patients,” says Hartwig.