When cancers of the intracranial compartment are difficult to access or remove through open surgery, laser interstitial thermal therapy (LITT)—a relatively new advancement in minimally invasive brain surgery—may be an option for patients with primary brain tumors or metastases.
Duke is one of the top-volume centers in the United States to offer this MRI-guided laser ablation procedure, which uses targeted doses of laser heat to treat recurrent, deep, or otherwise inaccessible lesions in the brain.
Peter E. Fecci, MD, PhD, a Duke neurosurgeon and LITT expert, explains that LITT can be especially effective in cases of recurrent brain metastases, radiation necrosis, deep-seated glioma, and odd lesions in the hypothalamus, such as a hypothalamic hamartoma.
“If you can safely do biopsy, then you can often do the LITT procedure,” says Fecci, who recently treated his 100th patient with LITT. “A lot of times, when tumors recur in the brain, patients may be told that surgery or treatment isn’t possible, but at Duke, we have helped lead and develop safe and effective treatments, techniques, and procedures that other places may not know about or say can’t be done.”
How LITT works to ablate lesions in the brain
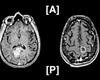
The procedure involves using a cooled laser probe to deliver a targeted and lethal dose of laser energy directly into the tumor. The NeuroBlate® System (Monteris Medical: Minneapolis, MN) employs robotic control, directional laser technology, real-time MRI-thermometry, and navigation software that enables the neurosurgeon to precisely ablate the affected areas.
Fecci explains that in order to kill a tumor, the stereotactically guided laser energy must be equivalent to 43°C for 10 minutes, which expands to an area approximately 1.5 cm from the laser. This coverage would be sufficient for a tumor that is 3 cm in diameter, he says, but if you drop more than one trajectory to heat a larger lesion, brain swelling becomes a concern.
“As we’re attempting to sculpt the lesion, we're constantly watching in real time in our intraoperative MRI suite, which tells us where the heat is going,” he says.
Latest research advancements
Fecci says that Duke has invested heavily in becoming one of the leading centers to advance the technology for LITT. One such technological advancement is the development of specific nanotechnologies that can act as “lightning rods,” expanding the laser treatment coverage by conducting heat more efficiently than normal tissue, Fecci explains.
Due to the non-uniformity of specific heat across different tissues (i.e., tumor, surrounding white and gray matter, regional heat sinks), this novel technology could make a significant difference in patient outcomes when LITT is employed for larger intracranial tumors.
“The nanotechnology enables us to heat and sculpt larger lesions much more quickly, thereby reducing the potential for swelling,” Fecci says.
Working in collaboration with Tuan Vo-Dinh, PhD, a Duke biomedical engineer, Fecci has been testing the Duke-produced nanoplatform in mouse models and artificial brain phantoms. Fecci and Vo-Dinh co-authored an October 2019 article in Immunotherapy outlining their investigation into the novel use of the laser-induced, nanoplatform-mediated photothermal therapy and checkpoint blockade immunotherapy for the treatment of glioblastoma in a murine model.
LITT vs. open surgery
There are several major advantages to performing LITT over open procedures. In addition to providing smaller incisions and faster hospital stays and recovery times, the laser heat synergizes with immunotherapy, working with the immune system to enhance the therapeutic effects, Fecci notes.
“After the laser procedure is completed, the blood-brain barrier tends to be open for a period of about four weeks, so it can increase vascular permeability for other treatments such as chemotherapy and immune infiltration and provide better access into the tumor,” he says.
As LITT requires only a 1 cm incision, most patients return home the same or next day with minimal pain. However, Fecci explains that the appropriateness of LITT depends on the size and location of the tumor. For example, patients with tumors larger than 3.5 cm or those located around the posterior fossa or cerebellum would likely not be good candidates for the procedure.
“LITT is not meant to replace open surgery all the time. It's meant to replace it in certain instances where the safety of an open surgery is potentially less clear, but you still really want to have an option for cytoreduction so that other therapies will work better,” he adds.
For more information or to refer a patient, visit:
https://www.dukehealth.org/treatments/neurosurgery/laser-interstitial-thermal-therapy