Neurophysiologic Intraoperative Monitoring May Be Feasible During Laser Interstitial Thermal Therapy
In a case report published in the August 1, 2016, issue of Journal of Clinical Neurophysiology, Duke investigators demonstrate the feasibility of using intraoperative neurophysiologic monitoring during laser interstitial thermal therapy to monitor epileptiform activity. The report describes the first 2 patient cases in which intraoperative electrocorticography monitoring was successfully used to record mesial temporal spike activity before and immediately after thermal ablation of the mesial temporal region.
Although craniotomy with resection is still considered the gold standard therapy for drug-resistant focal epilepsy, laser interstitial thermal therapy has in recent years provided a minimally invasive alternative, particularly for medically refractory mesial temporal lobe epilepsy (MTLE).
In general, the procedure is accompanied by shorter hospitalization times, lower complication rates, and potentially lower rates of long-term neurocognitive morbidity. However, seizure-free rates may be lower, possibly because of the current limitations on the use of intraoperative monitoring during laser interstitial thermal therapy. The ability to use neurophysiologic intraoperative monitoring to identify epileptogenic tissue and guide tissue ablation during laser interstitial thermal therapy may therefore improve patient outcomes.
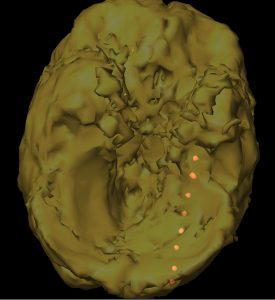
The report describes 2 patients with intractable MTLE who underwent magnetic resonance imaging–guided laser interstitial thermal therapy administered with depth-electrode electrocorticography (Figure). Both patients exhibited a marked reduction in seizures, accompanied by a reduction in discharges following ablation as recorded by electrocorticography.
“In the right setting, electrocorticography can be a powerful tool, and this is a novel implementation,” says Matthew W. Luedke, MD, epilepsy specialist and first author on the report. “We have shown that we can use electrocorticography during laser interstitial thermal therapy. The next step is to figure out what those electrocorticographic findings mean. This report lays a foundation for more exploration.”
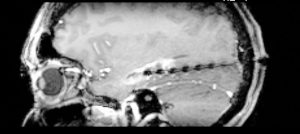
FIGURE. Sagittal magnetic resonance imaging showing the burnt lesion and probe (black dots)
As a follow up to the report, Luedke and his colleagues Saurabh R. Sinha, MD, PhD, neurologist, epilepsy specialist, and senior author on the report, and spine and neurosurgeon Michael M. Haglund, MD, PhD, will be conducting a prospective trial at Duke that will examine the safety and efficacy of neurophysiologic intraoperative monitoring during laser interstitial thermal therapy for patients with MTLE.
The study will assess the safety of neurophysiologic intraoperative monitoring and determine whether epileptiform discharge data recorded before and after laser interstitial thermal therapy are representative of seizure outcomes. The investigators seek to determine whether the use of neurophysiologic intraoperative monitoring during laser interstitial thermal therapy can aid prognostication and guide surgery, potentially improving seizure-freedom rates.
“Laser interstitial thermal therapy is accepted and currently being used in the clinic for epilepsy treatment—it’s a great option for the right candidate,” says Sinha. “But we hope to go one step further: We want to determine whether we can use neurophysiologic intraoperative monitoring during laser interstitial thermal therapy to predict the outcome in a patient and, ultimately, improve outcomes for patients with epilepsy who undergo laser interstitial thermal therapy.”