A 2024 report published by the Heart Failure Society of America projected the prevalence of heart failure (HF) to rise in the United States by 30% by 2030. “There’s a very heavy burden of HF in our society, and it continues to be the leading cause of death,” says Duke Health heart surgeon Jeffrey E. Keenan, MD, surgical director for mechanical circulatory support.
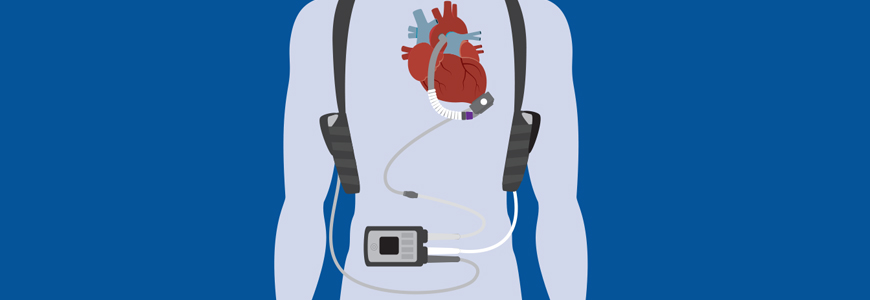
Heart transplantation remains the gold standard of treatment for advanced end-stage HF, but it isn’t always a viable option. Left ventricular assist devices (LVAD) represent an alternative treatment option for end-stage HF patients that may or may not be heart transplant candidates.
“I think that physicians underestimate who we could potentially manage successfully with LVAD and transplant,” says Keenan. “What’s happened in the last five to 10 years is really remarkable.”
LVAD advances
The advances in LVAD technology have made the devices a viable treatment to increase life span for patients with HF. These improvements have also made LVADs an option for more patients than ever before. “We now have better capabilities of transplanting or implanting LVADs in sicker and more marginal candidates, and we’ve done that while maintaining good outcomes,” Keenan says. “Many times, we can turn a patient around and give them a pathway to long-term survival with high quality of life.”
LVAD technology progressed significantly with the HeartMate 3 (Abbott Laboratories, Abbott Park, IL) model (HM3), which was tested at centers including Duke. The median survival on HM3 has now surpassed seven years. “Without this technology, this patient population would probably measure their remaining life span in months,” says Keenan.
The HM3 has performed so well that other competitors were driven out of the market, slowing innovation in the space for many years.
Testing a new generation of LVADs
Trials are now underway for a new generation of LVADs. The INNOVATE Trial, testing the BrioVAD system (BrioHealth Solutions, Burlington, MA), has completed the initial safety phase. Duke was one of eight sites to offer these first devices. “We’re very excited to participate in the trial,” says Keenan.
While both feature the fully magnetically levitated centrifugal pump technology to provide continuous blood flow, the BrioVAD offers several potential improvements over HM3:
- Smaller pump housing, which is easier to fit into the pericardium without distorting the ventricle
- More efficient blood path through the pump, offering similar flow levels at lower impeller speeds, potentially reducing blood shear stress and improving biocompatibility
- Smaller and more flexible driveline, potentially reducing infections. “Driveline infections remain one of the biggest challenges encountered with the HM3,” Keenan explains.
- Lighter controller and batteries to facilitate patient mobility and function
The first BrioVAD at Duke was implanted in March 2025, and three more have been placed since. “So far, our experience has been very promising,” says Keenan. “Most patients we approach for the trial are quite interested, and for those who’ve received the BrioVAD, they’ve responded well.”
Spectrum of HF therapies
For acute or temporary needs, Duke offers a range of circulatory support options, from inotropic infusions to extracorporeal membrane oxygenation (ECMO) to temporary, catheter-based LVADs such as Impella 5.5 (Johnson & Johnson MedTech, Danvers, MA). “We use these options to stabilize patients in acute shock or as a bridge to LVAD or transplant,” Keenan explains. “We have the capacity and ability to support shock and acutely decompensated patients with these temporary devices in a way that we didn't have five years ago. It’s been a game changer.”
Multiple studies have shown improved outcomes for patients at high-volume centers, and Duke is one of the few centers to perform a high volume of both LVAD and transplantation, leading the country in 2024 with 88 durable VADs and 132 heart transplants. This expertise gives patients more options and enables Duke physicians to select the therapy best suited for each patient.
“We think about treatment paths from all angles,” says Keenan. “We’ve accumulated a high level of experience and expertise throughout all levels and specialties within the team. I truly believe no one’s doing it quite the way we’re doing it.”
Recent technological advances could change the treatment paradigm for referring providers, Keenan concludes. “We want referring providers to feel empowered to reach out. We can do a lot more than we could 10 to 15 years ago. Never assume a patient is beyond help.”