With more than 350,000 coronary artery bypass graft (CABG) operations performed annually according to the American Heart Association, it is the most common cardiac surgery performed in the United States. Still, CABG via sternotomy is not appropriate for all patients who may benefit from surgical revascularization. Minimally invasive CABG (MI-CABG) offers a sternal-sparing approach to surgical revascularization of the left anterior descending artery (LAD) with robotic-assisted left internal mammary artery (LIMA) harvest via a small thoracotomy. The approach is gaining momentum nationally and now accounts for about 10% of CABG performed.
Robotic-assisted MI-CABG can be performed without cardiopulmonary bypass and without stopping the heart. Duke Health heart surgeon Brittany Anne Zwischenberger, MD, says MI-CABG expands the armamentarium of revascularization techniques for an aging population with an increasingly complex comorbidity profile. “Robotic-assisted, minimally invasive CABG has an important role in matching revascularization strategies to individual patients,” Zwischenberger continues. “It’s not competing with PCI or sternotomy CABG but offering an alternative to patients.”
Thoracotomy reduces risk, increases access
MI-CABG offers a surgical revascularization option for patients with comorbidities that increase risk of sternal wound infection or limit rehabilitation potential after sternotomy, including those with:
- Frailty or malnourishment
- History of lower extremity amputations
- Wheelchair or walker dependence
- Poorly controlled diabetes
- Large pendulous breasts with other risk factor for wound infection
- Current smoking status
- Immunosuppression
MI-CABG eliminates the risk of mediastinitis, which carries a high morbidity. Using the robot further reduces the thoracotomy incision size and wound infection risk.
Zwischenberger describes Duke’s protocol as “fast-track CABG.” “Most patients,” she says, “are transferred to the floor the same day of surgery and then discharged home on post-operative day three. With no sternotomy precautions, patients can return to full mobility in two weeks.” Multiple studies indicate MI-CABG is associated with significantly reduced recovery time, including reduced ventilator time, ICU stay, overall hospital stay, and time to full functionality. Patients are also less likely to receive blood transfusion.
Patients who may especially benefit from a faster recovery include those with:
- Stage 4 chronic kidney disease (CKD)
- Significant carotid disease
- Porcelain aorta
- Cirrhosis
- Relative contraindications to full anticoagulation including recent stroke or GI bleed
- Age 80 to 89
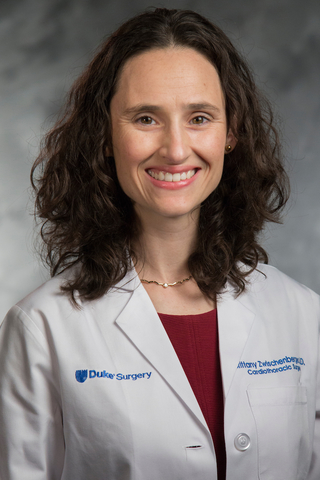
Opening up more options
While MI-CABG is an option for isolated LAD disease, it can also be used to treat multivessel disease in a hybrid approach. The LAD is treated surgically with MI-CABG, and the other vessels can be treated with percutaneous coronary interventions (PCI). The timing of PCI depends on the coronary artery disease pattern and patient presentation. Through a collaborative effort within the Duke Heart & Vascular team, Zwischenberger has worked closely with interventional cardiologist Andres M. Pineda Maldonado, MD, and Taylor M. Honeycutt, MHS, PA-C, to identify how the hybrid program can offer durable revascularization options to individual patients.
Patients with multivessel disease who are Black, Hispanic, or female of any race demonstrate worse outcomes after CABG or PCI yet are historically underrepresented in revascularization studies. A Duke team led by Zwischenberger and Pineda is a top enroller for the RECHARGE trial, which randomizes these patients with multivessel coronary artery disease to multivessel PCI or sternotomy CABG. Zwischenberger has additionally launched the RECHARGE Hybrid Registry of female, Black, and Hispanic patients who undergo hybrid revascularization. The goal is to capture objective outcomes as well as quality of life metrics over two years.
Revolutionizing heart surgery
While MI-CABG techniques have been described for decades, integration has lagged behind the innovation. “MI-CABG requires comfort with robotic mammary harvest and off-pump or beating heart coronary anastomoses, which are uncommonly taught in training,” Zwischenberger says. In the U.S., MI-CABG recently experienced renewed interest with a 17.6% increase in 2023 from the previous year. Still, only 144 centers perform robotic-assisted CABG, with most cases performed at high-volume centers.
For patients requiring revascularization who may not be a candidate for standard CABG, Zwischenberger encourages considering MI-CABG and a hybrid approach. “Our goal is to expand the options of revascularization,” says Zwischenberger. “Each patient should be considered for all the options we can offer, including PCI, MI-CABG (LIMA-LAD only), hybrid, and sternotomy CABG. By identifying the most appropriate revascularization strategy, we can deliver the highest quality of care to our increasingly complex patient population.”