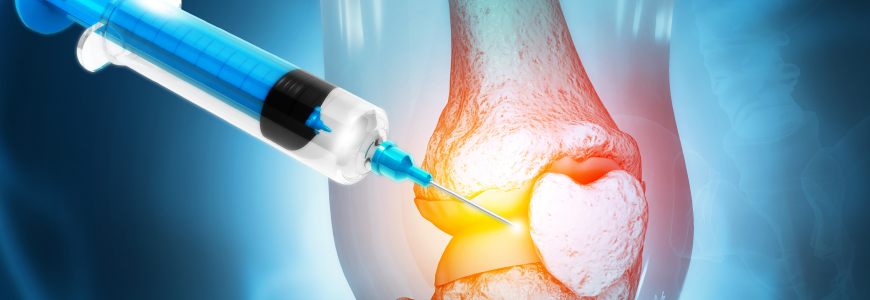
Research-based orthobiologic injections offer patients an option to aid recovery if conservative treatment fails. “The concept is to augment your own healing potential, harness the cells that you have for regular healing and concentrate them where the injury was,” explains Duke Health sports medicine specialist Blake R. Boggess, DO.
“Orthobiologics can jump-start the healing process from within,” agrees sports medicine specialist Harry C. Stafford Jr., MD, MBA, associate director of the James R. Urbaniak, MD, Sports Science Institute and director of Duke sports performance. “They bring platelets and growth factors into the area that subsequently can call in stem cells and other factors to influence healing.”
Although insurance companies typically do not cover orthobiologic injections, Boggess and Stafford stress that Duke strives to make treatments accessible to those who need them.
Learn how to refer a patient to Duke Orthopaedics.
Advancing orthobiologic care
Boggess has contributed to research published in the American Journal of Sports Medicine examining differences in how patients respond to various types of orthobiologic injections based on patient age and sex.
The study compared corticosteroid injections (CSI) to three cell-based therapies: bone marrow aspirate concentrate (BMAC), stromal vascular fraction (SVF), and allogenic umbilical cord tissue for age-based knee osteoarthritis (OA). BMAC had the highest percentage of response, and male patients responded more favorably to BMAC and SVF over other therapies, while women had better response to CSI than men.
“We’re still trying to explain why these different groups responded so differently,” says Boggess. “We want to look at whether the degree of OA has a stronger effect on treatment than age and sex.” He highlights that Duke’s Benjamin A. Alman, MD, is directing the federally funded NITRO study to research OA therapies to rebuild bones and joints to continue to advance the field.
Orthobiologic injections can also play an important role for athletes’ recovery from injuries, says Stafford. “We use them to complete the process in times when athletes have failed to fully recover from an injury to tendon, muscle, or bone with standard treatment.” He stresses that physical therapy (PT) and continued support are vital to recovery: “Athletes are in excellent physical shape, but they also have people managing their continuing care, therapy, and diet.”
Locations
- Duke Orthopaedics Arringdon (Morrisville): platelet-rich plasma (PRP), stem cells
- James R. Urbaniak, MD, Sports Sciences Institute (Durham): PRP
- Duke Sports Medicine and Orthopaedics Cary: PRP
Physicians
- Blake Boggess, DO
- Anthony S. Ceraulo, DO
- Luting S. Eckensweiler, DO
- Stephen P. Shaheen, MD
- Harry Stafford, MD, MHS
- Rebecca Wadlinger, DO
Why Duke
Duke Orthopaedics offers options for care at all levels. For patients with OA of the hip, knee, shoulder, or carpometacarpal joints, Duke’s Joint Health Program offers comprehensive care managed by primary OA providers. Boggess cites the program as the first place to refer patients with OA. “If that treatment doesn’t work, we can look at hyaluronic gel injections or orthobiologics before we jump to surgery,” he says.
“We have the full gamut, from basic science research to total joint replacement and everyone in between, all working together in interdisciplinary conferences,” Boggess continues. “We have people who specialize in each joint. We offer the full scale of options.”
Stafford concurs: “Duke is an elite place for musculoskeletal care. No matter what injury or problem your patients have, we have experts that will help them.”