An evaluation system that assigns a score to Type 2 systematic lupus erythematous (SLE) symptoms is being implemented by the Duke Lupus Clinic as the most recent step in a novel initiative to measure and quantify SLE disease by combining the findings from patient questionnaires and physician evaluations.
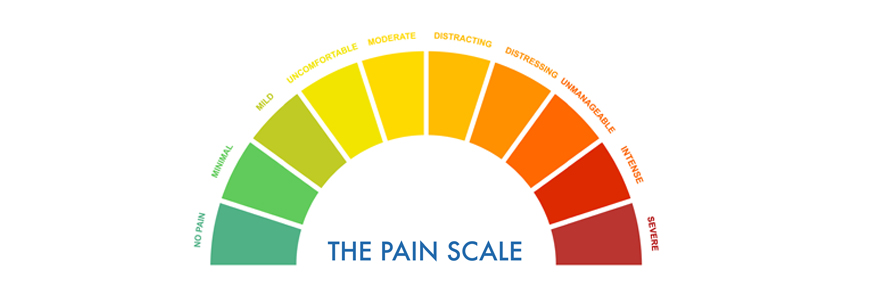
The Type 2 Physician Global Assessment (PGA) score system, based on a three-point visual analog scale reported by physicians, has been implemented into routine clinical care in the Duke Lupus Clinic, says Jennifer L. Rogers, MD, director of the clinic. The Type 2 PGA is the physician’s overall assessment of Type 2 SLE symptoms: fatigue, widespread pain, sleep disturbance, brain fog and mood disorders.
By using a specific Type 2 PGA, similar to the traditional PGA score used in lupus clinical trials for overall SLE activity, rheumatologists are reminded to address these often difficult-to-treat SLE symptoms. While the assessment process is underway, the clinic’s rheumatologists and researchers are finetuning patient-reported outcome measures to continue building a comprehensive disease database as part of the Duke Lupus Registry.
The effort to create precise SLE symptomology definitions—the first such effort in American rheumatology—helps address discordance between patients’ perceptions of lupus symptoms and physicians’ assessment of disease activity, Rogers says.
The team published a summary of the new SLE classification system and efforts to create a more precise subtyping effort in Arthritis Care & Research in 2018. The categories are designed to help identify and treat the markedly varied presentations of SLE with more precise therapies. In addition to Rogers, the authors included colleagues Megan E. B. Clowse, MD, MPH, Lisa Criscione-Schreiber, MD, MEd, and David S. Pisetsky, MD, PhD.
Incorporating Patients' Lupus Experiences
Rogers and colleagues in the clinic, one of the busiest in North Carolina, have been integrating the SLE subtype categories into daily practice with the goal of more effectively incorporating patients’ lupus experiences and ensuring that all SLE symptoms are heard and addressed.
The Duke Lupus Clinic research team includes Rogers, Clowse, Pisetsky, Criscione-Schreiber. Kai Sun, MD, MS, Jayanth R. Doss, MD, MPH, Rebecca Sadun, MD, PhD, and Amanda Eudy, PhD, are collaborating to continue developing the categorization model.
The broad SLE subtypes defined in the research are Type 1 and Type 2 SLE; however patients present with varying degrees of Type 1 and Type 2 features, often forming clusters symptoms, which may fluctuate over time. The symptoms of the various types are defined below:
- Type 1 SLE: Autoimmune-mediated SLE symptoms characterized by inflammation or organ damage which can respond to immunosuppression. Symptoms include lupus nephritis, inflammatory arthritis, cutaneous rash, serositis, mucocutaneous ulcers, alopecia, vasculitis, myositis, hematologic abnormalities, neuropsychiatric lupus, lupus enteritis, Interstitial lung disease, and shrinking lung
- Type 2: Non-inflammatory symptoms that do not respond to standard immunosuppression therapies. Symptoms include fatigue, widespread diffuse pain, cognitive dysfunction, sleep disturbance, and mood disorders such as depression, and anxiety.
- Mixed Active SLE: A combination of Type 1 and Type 2 symptoms.
“Interestingly, we found Type 2 SLE symptoms affect lupus nephritis patients less often than non-nephritis patients,” Rogers says. “As a result, we are planning future projects to delve deeper into clinical, laboratory, demographic, socioeconomic and transcriptomic differences between patients with the Type 1 vs Type 2 SLE symptoms in order to better understand the mechanism driving these symptoms.”
Rogers says the Duke Lupus Clinic team plans further study of the symptom clusters and the ways in which the clusters change over time.