After years of partnering to treat aortic patients, Duke’s Divisions of Cardiothoracic Surgery and Vascular Surgery are officially collaborating in the Duke Center for Aortic Disease. “A more formalized relationship allows us to build more infrastructure, expert research, and multidisciplinary care,” says vascular surgeon Chandler Long, MD, center co-director.
Co-director G. Chad Hughes, MD, section chief of Aortic Surgery, agrees: “This new push will help us to expand teaching, imaging capabilities, and clinical services.”
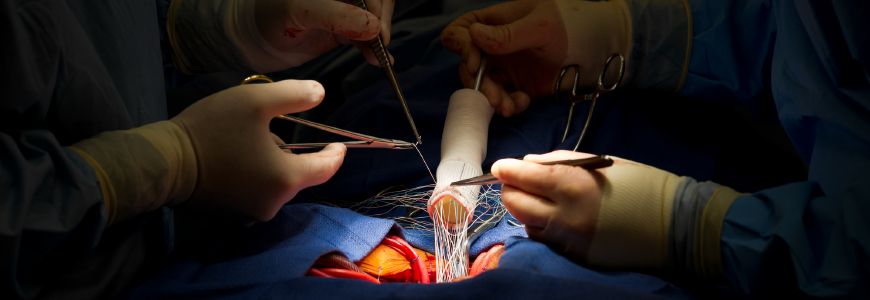
The center focuses on the aortic vessel from the aortic valve to the iliac bifurcations. The equal partnership and longstanding collaborative relationship between cardiothoracic and vascular specialists uniquely position the center to provide advanced care for dissections, aneurysms, and other aortic conditions and anomalies. Opening a third hybrid operating room at Duke has also increased the number of patients the center can treat, decreasing wait times.
Leading the way
The Duke Center for Aortic Disease offers advanced care with expert faculty in all areas. “Many institutions with aortic centers are strong in either cardiothoracic surgery or vascular surgery, and their treatment algorithms tend to funnel patients in one direction,” says Long. “We are strong in both areas and collaborate well, allowing us to offer a comprehensive, patient-centric solution based on a broad, multidisciplinary skillset. Our collaboration sets us apart from anyone on the East Coast.”
The center seeks to improve treatment now while advancing the future of aortic medicine. “Education is an important pillar to the aortic center. We hope to expand the existing aortic fellowship to both cardiothoracic and vascular surgery trainees, creating aortic-trained surgeons that can treat and provide access to a broader scope of patients. This training paradigm doesn’t exist anywhere else in the country,” says Long. The center will also focus on advancing aortic research within both translational and clinical outcome pathways. “The aortic center’s global mission is multifaceted, and we cannot understate the importance of preventative medicine with regard to aortic pathology,” he adds.
Detecting aortic conditions
Although aortic conditions are commonly caused by high blood pressure, most don’t show symptoms. “A lot of aneurysms and dissections are preventable,” says Hughes. “In many cases, this is a disease of the medically underserved. Had these individuals had access to a primary care doctor when they first developed high blood pressure, many of these conditions could have been prevented.” Hughes supports efforts for community screening for hypertension and aneurysms. “If we can get blood pressure and other risk factors under control, we decrease aortic disease, which is important since some conditions, such as aortic dissection, may present as sudden death.”
Connective tissue disorders are another risk factor for aortic conditions. Syndromes including Marfan, Loeys-Dietz, and Ehlers-Danlos can weaken the vessel’s layers, leading to dissection. All first-degree relatives of a patient with aortic disease should be screened, but not all genetic disorders are inherited. “Twenty-five percent of Marfan cases constitute a new mutation,” says Hughes. “It’s hard to screen for that, so we’re always trying to raise awareness.”
Patients should be referred to the center with any of the following:
- hereditary thoracic aortic disease (or in a first-degree relative)
- thoracic aortic aneurysm of 4 cm or larger
- abdominal aortic aneurysm of 3 cm or larger
Patients with smaller aneurysms or who have previously had a repair can also be referred for the center to follow.
The Duke difference
Research shows that centers that perform a high volume of surgeries cut the risk of death during aortic repair in half versus other facilities. Dedicated aortic surgeons’ mortality outcomes are almost threefold better than other surgeons’ for open repair of acute type-A dissection. Led by Duke Chief of Cardiology Manesh Patel, MD, and Sreek Vemulapalli, MD, of the Duke Clinical Research Institute, the IMPROVE-AD study is currently investigating the best management for uncomplicated type-B dissection, with NIH funding. Hughes and Long lead the Duke site of the study.
“We have the surgical expertise to deal with everything from the aortic valve to the peripheral vasculature with high-volume surgeons who have great results,” says Hughes. “We have the infrastructure to follow patients and give support for lifelong follow-up.”
The multidisciplinary team also contributes to the center’s success: “We have outstanding teams for cardiovascular anesthesia, imaging, genetics, and more,” says Hughes. “We coordinate care for patients across all their needs within the hospital system.”
“We’re really trying to build engagement in the community,” says Long. “We want to meet patients where they are and develop relationships with community providers. When it comes to referral, the answer for us is always, ‘Yes, we’ll take them.’”