Some patients with esophageal motility and reflux disorders may not be candidates for a major surgery or may wish to avoid surgical intervention altogether, opting instead to manage their chronic symptoms with medication and lifestyle changes. However, a host of third-space and other minimally invasive endoscopy procedures at Duke give patients with a broad range of gastroenterological conditions—including reflux, achalasia, Zenker’s diverticulum, and esophagogastric junction outflow obstruction—a plethora of nonsurgical options to consider.
In this Q&A, Duke gastroenterologists M. Stanley Branch, MD, and Darin L. Dufault, MD, highlight some of the highly technical endoscopic procedures that can improve a patient’s quality of life.
Q: What has been the standard of care at Duke for esophageal motility disorders?
Branch: We’ve been doing the peroral endoscopic myotomy (POEM) procedure for several years, which involves making an incision in the esophageal wall and creating a tunnel inside the submucosa to open up a space through which to access the area of esophageal muscle that is not relaxing properly. Most patients are wanting to go this route when they hear about it because there’s no external wound to heal from and they can go home the next day. POEM allows us to treat a broader span of esophageal muscle than major surgery, so for certain subsets of patients, it’s probably more effective.
Q: Which newer esophageal procedures are becoming the most effective alternatives to surgery in this space?
Dufault: Aside from POEM for motility disorders, one of the more cutting-edge techniques we’re using is the transoral incisionless fundoplication procedure, which reconstructs a patient’s anti-reflux valve to provide relief from acid reflux disease. In addition to primary care providers, community dentists, pulmonologists, and otolaryngologists see these patients all the time, usually presenting with aspiration issues, chronic cough, vocal cord problems, and halitosis, all of which could possibly be related to uncontrolled reflux. Additionally, we are also performing endoscopic submucosal dissection to remove large, complex lesions from anywhere in the GI tract. This endoscopic technique has the potential to remove precancerous polyps or even early cancer. Lastly, for highly specific cases of complete esophageal obstruction, we also specialize in peroral endoscopic tunneling for restoration of the esophagus (known as POETRE).
Q: Which procedure is growing fastest among the geriatric patient population?
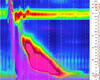
Branch: We’re seeing more and more cases of Zenker’s diverticulum, which is when the hypopharynx is not relaxing properly and a thickened septum develops, causing a pouch to form that traps food and fluid. To treat this condition, we’ve been doing a Z-POEM procedure to dilate the mucosa and perform a myotomy on the affected muscle endoscopically. A new high-resolution motility testing we have at Duke has helped us to define the subtleties to make the diagnosis, especially for patients with a condition that had been previously labeled as a functional gastrointestinal disorder.
Q: Why would you choose to perform Z-POEM over surgery in certain cases?
Branch: Performing Z-POEM in appropriate cases is a little safer and potentially more efficacious, according to our initial data. However, one of the problems we run into with Z-POEM is that you can’t always know how deep the esophageal sphincter is in order to cut down the length of the pouch, so without careful selection, a revision procedure could be needed to treat all the muscle.
Q: What potential benefits are there for patients with reflux who undergo these types of endoscopic procedures?
Dufault: So many patients are on proton-pump inhibitor medications, with more than $11 billion a year spent on reflux medications in the U.S.—it’s a tremendous financial burden. Even for patients who continue acid medication after the procedure to fully manage their reflux, we are often able to reduce their symptoms and/or reduce the amount of medication they take. There is a lot of research potentially linking long-term consequences to being on this type of medication, so to be able to reduce their dose or eliminate it entirely is beneficial for the patient’s long-term health. With some of the nonsurgical options we offer at Duke, we can help patients who are curious about what they can do to get off these medications, short of surgery.