Müllerian ducts must undergo specific changes during fetal development to form the mature female reproductive tract. When they do not properly develop, Müllerian anomalies may result. Some anomalies are present at birth, but many are not discovered and addressed until much later in life. Duke’s Müllerian Anomalies Program brings together a multidisciplinary team representing pediatric, adolescent, and adult medicine to offer patients the full spectrum of care from proper diagnosis to innovative treatments.
“These conditions require lifespan care,” says Cassandra K. Kisby, MD, MS, urogynecologist. “Our program, the Genitourinary Congenital Anatomic Differences Program, also called the GU CARES Program, has the level of expertise to offer patients options that optimize long-term health, function, and quality of life.”
For Müllerian anomalies discovered prenatally, expecting parents may have consultations during pregnancy to understand the severity of the condition and potential corrective interventions. “Sometimes we recommend waiting on surgical correction, or patients require multiple surgeries over time. That’s why it’s critical to have multiple specialties working together to consider the best option for the patient now and in the future,” says Kisby.
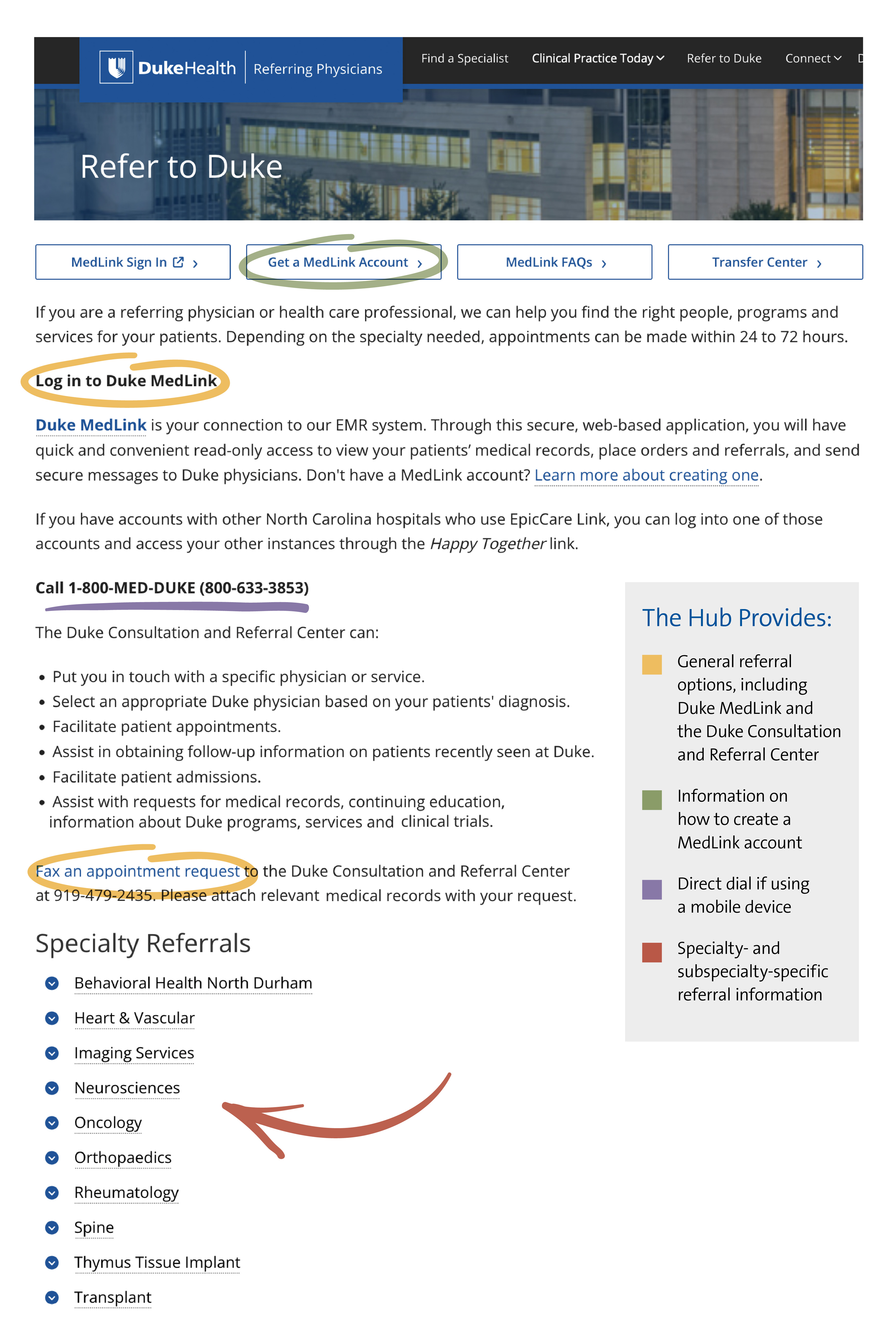
To refer a patient to the Müllerian Anomalies Program, call 919-401-1000 or 919-684-2471. Internal referrals may be placed via the electronic medical record by ordering: Adult-Peds Congenital GYN/GU Abnormality Referral.
Lifespan considerations
Different concerns and symptoms arise as a child develops through adolescence and adulthood, as they consider fertility, sexual function, and family planning. With collaboration between urologists, colorectal surgeons, and pediatric and adolescent gynecologists, the team reviews each case to determine the safest and best treatment pathway. This can include vaginal dilation, vaginoplasty, vaginal septum surgery, uterine surgery, urinary system surgery, and pelvic floor physical therapy.
“Often in these cases, patients don’t expeditiously get answers for why they have pain until they come to a provider who has extensive experience with diagnosing and treating it,” Kisby says. “It’s important for providers to know to look for issues with the kidney, bladder, and urethra, which can form congenitally along with the Müllerian anomaly.”
The related conditions that Duke experts treat include:
- Vaginal anomalies: vaginal agenesis (absence or partial absence), vaginal septum (longitudinal, transverse, or oblique)
- Uterine abnormalities: uterus didelphys (double uterus), arcuate uterus (curved), unicornuate uterus (one-sided), bicornuate uterus (heart-shaped), septate uterus (partitioned), absent uterus
- Mayer-Rokitansky-Küster-Hauser (MRKH) Syndrome: an undeveloped uterus and upper vagina with external genitalia that appear normal
- Obstructed hemivagina and ipsilateral renal anomaly (OHVIRA): including uterus didelphys, unilateral low vaginal obstruction, and same-sided absence or underdevelopment of a kidney
- Complex anomalies: cloacal exstrophy, bladder exstrophy, disorders of sex development (congenital adrenal hyperplasia, androgen insensitivity syndrome, sex chromosomal disorders)
Fostering psychological safety
A large focus of the program is managing the psychological impacts Müllerian anomalies and related issues have on patients. “They can be hard to process and manage as a young person. One of the first things we communicate to patients and their parents during our initial consultations is that they didn’t do anything to cause this; it’s fairly common. For example, vaginal agenesis occurs in one in 5000 births,” says Kisby.
The program works with colleagues from social work and psychology to extend resources for patients to grasp how their conditions affect them and how they will cope. Kisby says the team provides psychological safety to talk about it, find acceptance, and create a path forward that patients feel comfortable with.