The Duke Cancer Institute Thoracic Oncology Program is nationally recognized for its leadership in providing multidisciplinary and personalized approaches to detect and treat all types and stages of thoracic cancers, including less common malignancies such as esophageal cancer. With cutting-edge treatments, clinical trials, and surgical excellence, the team is driving innovation to improve patient outcomes, survival rates, and quality of life.
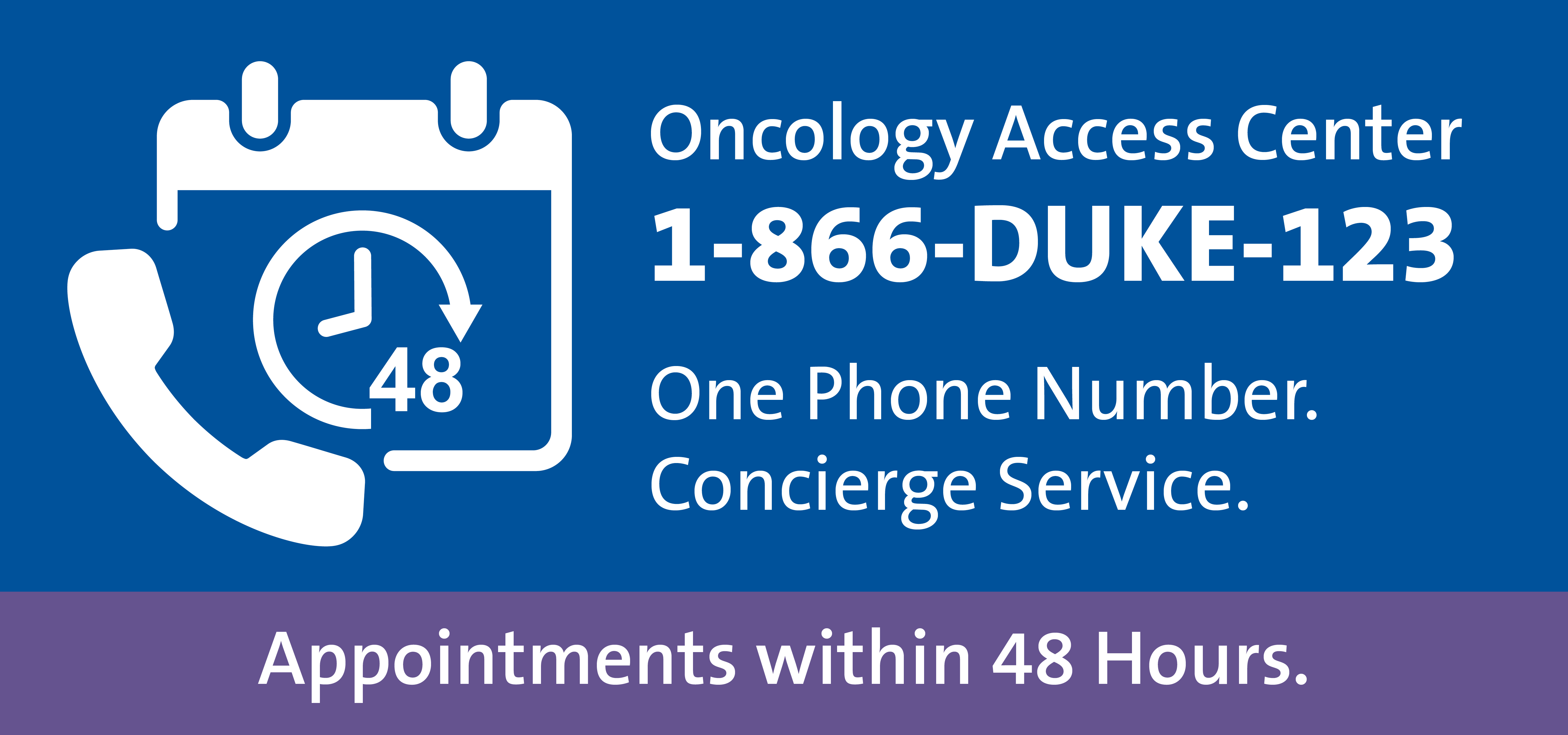
Call the referring provider team Monday through Friday between 8:00 a.m. and 4:30 p.m. at 866-385-3123 (1-866-DUKE-123). You can also email OncologyReferral@Duke.edu or fax 919-613-2316.
Focus on early detection
The Duke Health Lung Nodule Clinic leverages advanced imaging capabilities and a dedicated, experienced team to manage incidental nodules identified on imaging studies. Pulmonary nodules are common incidental findings on chest X-rays and CT scans of adults, appearing in approximately 50% of thoracic imaging studies. While most pulmonary nodules are benign, a small yet significant percentage require further workup. By identifying lung nodules early and assessing them, patients have a faster pathway to diagnosis and treatment if the nodule is cancerous.
The clinic is guided by the latest research, showing that following incidentally-detected indeterminate pulmonary nodules may lead to early detection of lung cancer when managed by a dedicated team, which is similar to that for patients undergoing low-dose CT scan lung cancer screening. For patients with confirmed lung nodules that require biopsy and removal, Duke’s thoracic surgeons and pulmonary interventionalists work closely to offer personalized management for patients.
These treatments can include procedures for both diagnostic and therapeutic purposes in the same sitting, such as robotic bronchoscopy and minimally invasive lung resections, speeding time to treatment and eliminating the need for multiple appointments and procedures that require anesthesia. “This is a transdisciplinary program with our interventional pulmonologists and thoracic surgeons collaborating pre-, during, and post-operatively,” says Betty C. Tong, MD, MHS, MS, thoracic surgeon and surgical oncologist.
Comprehensive treatment
The thoracic oncology team has expertise in treating the full range of cancers affecting the thoracic cavity, including lung and esophageal cancers. “We have a multidisciplinary approach, with the breadth of experts required for even the most complex cases,” says Tong.
For example, esophageal cancer treatment involves a close partnership between thoracic surgeons, medical oncologists, radiation oncologists, and gastroenterologists to develop comprehensive surgical and post-surgical treatment plans. Tong says that the program is unique in its subspecialty collaboration and advanced options for patients. “Our surgeons are some of the most experienced in performing minimally invasive esophagectomies, which result in a much quicker healing time and less potential surgical complications for patients.”
After surgery, patients are quickly connected to medical oncologists, radiation oncologists, and gastrointestinal cancer experts to continue their care and monitoring.
Additionally, the team has vast experience creating personalized approaches to treating every type and stage of lung cancer. Duke’s skilled surgeons have longstanding experience and expertise in minimally invasive techniques, including single-port robotic surgery for lung and mediastinal tumor resections. Other innovative lung cancer treatments at Duke include:
- Immunotherapy and targeted systemic therapy
- Photodynamic therapy
- Radiofrequency ablation
- Stereotactic radiosurgery
- Targeted radiation therapy
Expanding clinical trials portfolio
Many of the thoracic oncology team’s physicians are actively involved in trials studying new, promising lung cancer treatments. One example is a phase 3 study led by Tong exploring whether perioperative physical activity in older adults with lung cancer supports improved post-surgical outcomes. “We’re interested in more than just pharmaceutical or surgical indicators of better patient outcomes; this study examines exercise as ‘medicine,’” says Tong.
There are about 20 active clinical trials supporting thoracic cancer studies, examining new treatments for small cell lung cancer (SCLC), non-small cell lung cancer (NSCLC), and solid tumors from metastatic disease. Jeffrey Melson Clarke, MD, a medical oncologist, leads clinical trials for the Thoracic Oncology Program.
“If our community providers have a patient who is concerned about lung cancer risk, or who has been diagnosed with a lung nodule or any thoracic malignancy, we’re here to support with a second opinion, further diagnostic workup, or treatment planning. We have all the resources we need to deliver the best options for patients from diagnosis to survivorship,” says Tong.