To refer a patient to Duke neurosurgery, call 919-684-7777.
A 28-year-old female patient experienced weakness on the right side of her face, dysarthria, and numbness on her face and hand, with episodes occurring several times. This prompted an MRI, showing changes consistent with restricted blood flow in the left hemisphere and evidence of a stroke with deep white matter. Further imaging with an angiogram revealed diminished blood flow on the brain’s left side, confirming the diagnosis of moyamoya. The patient sought a second opinion from Duke neurosurgeon Erik F. Hauck, MD.
Hauck repeated MRI imaging, revealing changes on both sides of the brain. “We knew surgery was recommended for this patient, but we wanted to make sure the patient’s strokes were stabilized for at least four to six weeks to allow the vulnerable brain tissue to heal, minimizing complications and increasing bypass success,” says Hauck. The patient was prescribed low-dose aspirin and monitored until surgery was scheduled.
Question: How did Hauck approach the surgery to optimize results, recovery, and quality of life?
Answer: Hauck performed a complex bypass surgery to restore optimal blood flow in the left hemisphere. “Our goal with the procedure was to provide additional blood flow to the brain by creating a direct and indirect bypass at the same time. Blood flow would then grow based on the demand from the brain,” says Hauck.
While moyamoya is relatively rare, Hauck has been performing this procedure for over 20 years, completing 5 to 10 cases per year.
Hauck has a particular approach to minimize surgical scarring. “I focus on minimal hair shaving, which is very important for most patients. The incision is just a few millimeters wide, and after surgery, hair can be combed right over it. When it heals, you barely see the scar,” he adds.
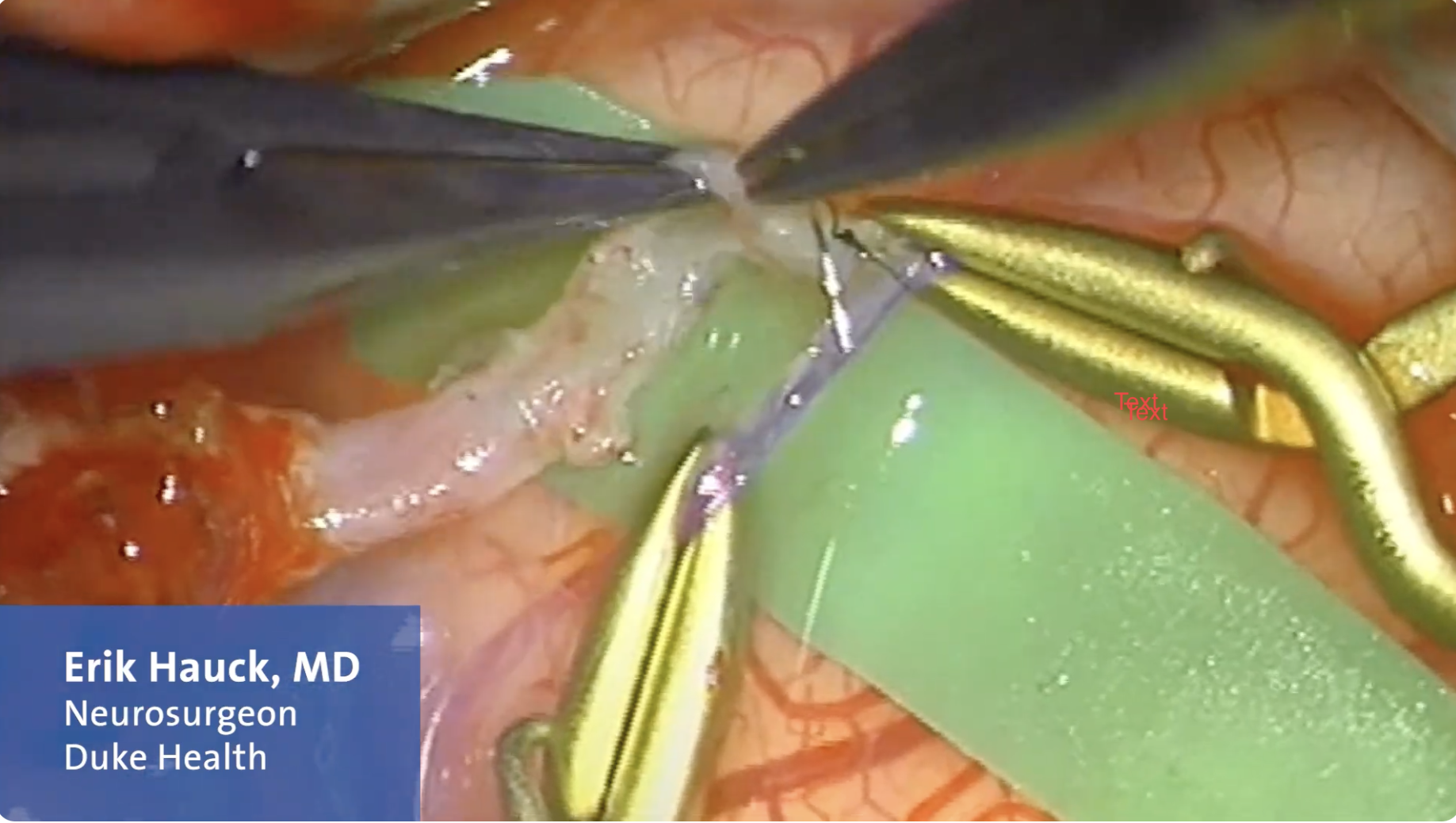
Hauck then finds the graft location. For this case, it was the superficial temporal artery (STA). He mobilized the branch of blood vessels that leads to the scalp and dissected the graft. This required moving the temporalis muscle to the side and making a one-inch incision to expose the small vessels on the surface of the brain’s temporal and frontal lobes.
After locating a good artery from the scalp and finding a favorable branch, he placed tiny clips on the vessels to temporarily stop the blood flow. He then made a small incision in the brain artery and connected the STA branch to the middle cerebral artery (MCA) with 15 super-fine stitches. “I use 15 to 20 sutures because more sutures support better approximation of vessel walls and allow anastomosis to grow over time,” says Hauck.
Then, Hauck checked the bypass and blood flow using Doppler to measure blood flow velocity and an angiogram to check vessel geography. “When we completed imaging, after surgery, we saw the areas of the brain previously affected by reduced blood flow begin picking up flow and changing in pigmentation,” explains Hauck.
Hauck also performed an indirect bypass at the same time, folding dura over to recover membranes that gradually generate new blood vessels to the brain to further improve blood flow.
After the procedure, the patient recovered in the ICU overnight, moved to the hospital floor the next day, and was discharged soon after. “The surgery was fortunately routine; everything went as planned, every step went smoothly, and the patient recovered well with optimal results,” says Hauck.
The patient was not local to Wake County, so Hauck collaborated with her local team to have her staples removed. Two weeks post-operative, she had a brief vasovagal event and presented to her local ER. “I talked directly to the ER physician, and we planned for her to be further evaluated by one of our neurologists, who confirmed it was an isolated syncope event and not a seizure or anything related to the surgery,” says Hauck.
The patient remained on low-dose aspirin and has been stroke-free. “We check her bypass every few months with imaging. Her blood vessels expanded five to six times larger compared to the time of surgery, and she hasn’t experienced any strokes,” Hauck says. “She is doing well and doesn’t have any restrictions on her daily life.”
Hauck notes that he is always available to his patients and referring physicians to discuss moyamoya cases and provide second opinions. “We have a team of neurologists and neurosurgeons who are very experienced in treating moyamoya. This is a rare condition, but it’s not rare for us as a destination center treating patients from all over the United States who travel for our unique experience,” says Hauck.
This video reviews the surgical bypass technique applied by Erik Hauck, MD, in this case.
