Call the referring provider team Monday through Friday between 8:00 a.m. and 4:30 p.m. at 866-385-3123 (1-866-DUKE-123). You can also email OncologyReferral@Duke.edu or fax 919-613-2316.
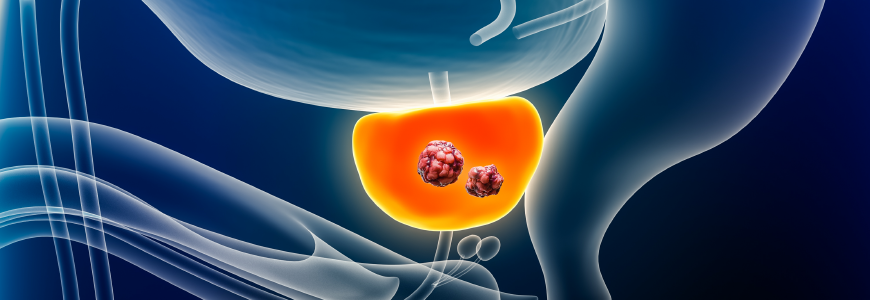
A 76-year-old man diagnosed with prostate cancer in 2008 underwent various treatments and had a local recurrence in 2012. He was treated with hormone therapy, brachytherapy, and cryoablation, but his prostate-specific antigen (PSA) rose again in 2013 when bone metastasis was detected. He continued on hormone therapy before seeking care at Duke Health with genitourinary medical oncologist Daniel J. George, MD, in 2015.
George started the patient on sipuleucel-T for metastatic castrate-resistant prostate cancer. “Despite localized and constitutional symptoms from his prior and ongoing cancer treatments, this patient was completely asymptomatic from prostate cancer, which made him an ideal candidate for sipuleucel-T. There are several underutilized treatments in the armamentarium against prostate cancer and sipuleucel-T, an autologous cellular immunotherapy, is one of them,” says George.
The patient continued with treatment and participated in a clinical trial at Duke, but in 2022, his PSA rose to 175 ng/ml.
What innovative treatment did Dr. George offer this patient?
The timing of this patient’s needs aligned with the 2022 FDA approval of a targeted radiopharmaceutical therapy for metastatic castrate-resistant prostate cancer. “Because Duke Health participated in a trial that led to the FDA approval of lutetium Lu 177 vipivotide tetraxetan (177Lu-PSMA-617), we were able to quickly expand this service to patients,” says nuclear medicine specialist Terence Wong, MD, PhD.
Unlike systemic chemotherapy or radiation, radiopharmaceutical therapies have a more tumor-targeted delivery, carry a lower toxicity profile, and are often better tolerated by patients.
The treatment is indicated in patients whose tumors bind to a radiolabeled probe used to image tumor targets with PET scans. Once identified, eligible patients can undergo treatment with a radionuclide therapy delivered by a similar molecular probe tied to a lethal dose of radiation. “We’re able to image the proposed molecular targets and treat them. When we image the tumor targets, not all tumors take up the radioactivity equally, so we have more insight into why targeted therapies may or may not be working,” says Wong.”
George suggested the patient be considered for 177Lu-PSMA-617, and engaged with Wong to review the case. “This treatment is given under close collaboration with our nuclear medicine experts; our teams work together to seamlessly manage the patient, which is not always the case at other centers,” says George.
The patient had a PSMA PET scan, which showed that his metastases would take up the radiopharmaceutical. He received his first dose in the fall of 2022 and followed the standard treatment course of six doses, six weeks apart. He was monitored closely before and after each treatment and tolerated them well. After the last treatment, his PSA level lowered to 10 ng/ml.
“This patient’s PSA dropped significantly without major side effects. He has had a long response, and did not require any additional treatment for the next nine months,” says George.
Expanding to more patients
The original approved use of 177Lu-PSMA-617 was for patients who already had chemotherapy. Recently, however, this has been expanded to include patients who have not yet had chemotherapy, allowing patients to be treated earlier in their disease process.
“We’ve seen a lot of patients respond well to radiopharmaceutical therapy for prostate cancer. We treat each patient as an individual. Not all patients respond as well as this case; sometimes we need to reassess the response by PET imaging. We then work very closely with Dr. Wong and his team in nuclear medicine to ensure that our patients receive the best and safest care possible,” explains George. The team is also examining how radiopharmaceutical therapy could be applied to treat additional cancers in the near future, further expanding access to more populations.
Duke is one of the first cancer centers in the country to become designated as a Comprehensive Radiopharmaceutical Therapy Center of Excellence. Duke’s Radiation Safety Division oversees all treatments. “Patients are prepared and instructed by this team, and they provide support to protect patients and staff against contamination and unnecessary radiation exposure. It’s one of the many moving parts of our process that deliver exceptional patient experiences,” says Wong.