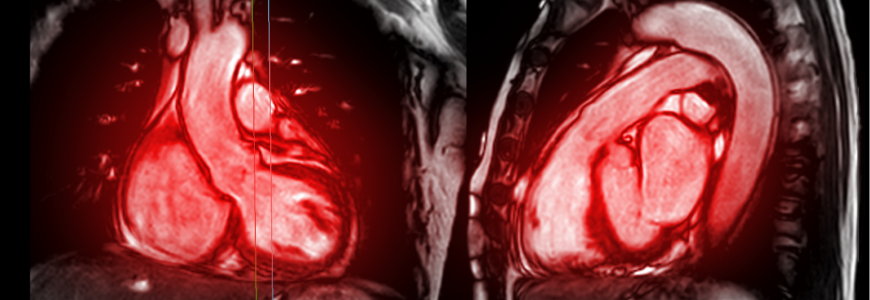
Duke’s precision cardiomyopathy program has pioneered a comprehensive approach to treat patients with cardiomyopathy. The cardiology department’s expertise combined with advanced cardiac imaging and genetic testing help Duke physicians identify the causes of cardiomyopathy cases, says advanced heart failure specialist Karen Flores Rosario, MD, who oversees rare and familial cardiomyopathies within the program.
“Having a hub for cardiomyopathies is important because that gives us more access to designated imaging teams as well as cardiologists and other specialists that help us build that network and provide that care for patients,” Flores says. The program also allows for better coordination with the Duke Cardiac Sarcoidosis and Cardiac Amyloidosis Programs, directed by cardiologists Ravi Karra, MD, MHS, and Michel G. Khouri, MD, respectively.
“Currently in the field, there’s a phenotype-first approach: a heart has to look like it has amyloid cardiomyopathy before physicians pursue workup,” Khouri says. “All current therapies are excellent, but they all work better if we diagnose earlier. We’re striving to improve early detection through precision approaches.”
Genetic causes of cardiomyopathy
Flores sees patients with non-ischemic cardiomyopathies and a family history of heart failure or sudden cardiac death as well as patients who recently had a family member diagnosed with a genetic form of cardiomyopathy and want to learn about their individual risk.
Flores cites experienced genetic counselors as a key part of the program. “About 30% to 40% of the disorders that cause dilated cardiomyopathy can be genetic,” says Flores. “Our genetic counselors help give appropriate pretesting genetic counseling to prepare patients for the nuanced results. They also help us get the desired testing, and we work together to provide recommendations for next steps.”
Helping patients now and in the future
In addition to providing cutting-edge care, Duke’s research seeks to better understand how cardiomyopathy develops. The TRACE AI study coming to Duke uses artificial intelligence to examine echocardiogram and ECG features to predict cardiac amyloidosis. “They’ve demonstrated a signal about two years before current diagnoses,” Khouri says.
The GENE-CARES study uses machine learning to examine imaging and electronic health records to identify patients with high-risk phenotypes to bring them in for testing and genetic counseling. The research effort OneDukeGen takes a genome-first approach, with the ACT-EARLY trial on medical prophylaxis in patients with confirmed genetic predisposition for transthyretin amyloid cardiomyopathy before possible symptoms.
If patients need advanced heart failure therapies in the future, “that’s something we can provide right here,” Flores says. Duke led the country in volumes in 2024, combining 88 durable VADs and 132 heart transplants, with expertise to care for all stages of heart failure. “Having all the resources to manage these conditions makes Duke unique,” Flores adds.