Congenital heart defects are the most common types of birth defects and a leading cause of infant illness and mortality associated with birth defects. But thanks in part to recent breakthroughs in transcatheter interventions, babies are living longer, healthier lives and avoiding the risks of neonatal surgeries.
Duke pediatric cardiologists are at the forefront of these innovations, successfully treating children of all ages—from extremely premature babies to young adults. Procedures are performed in Duke’s dedicated pediatric cardiac catheterization and electrophysiology labs, using the latest 3-D imaging systems and allowing the greatest precision and least amount of radiation.
Duke pediatric cardiologist and Vice Chief of Clinical Practice, Kevin D. Hill, MD, highlights three major breakthroughs in interventional catheterization that have changed outcomes for children in the past decade:
1 - Transcatheter Pulmonary Valve Replacement (TPVR)
Until the last decade, replacing a faulty pulmonary valve could only be achieved with open heart surgery; however, because all surgically implanted valves have a limited lifespan, patients faced the need for many surgeries during their lifetime. With TPVR, Hill explains, a compressed tissue heart valve is placed on a balloon catheter, advanced through the femoral or internal jugular vein to the heart, and positioned directly inside the diseased pulmonary valve. The balloon is inflated to expand the stent, and the valve is secured in place. The new valve immediately begins to work and can last as long as 15 years before needing replacement. The Duke team has performed TPVR on children as young 6 years old, as well as teenagers and young adults.
2 - Patent Ductus Arteriosus (PDA) Stent Placement
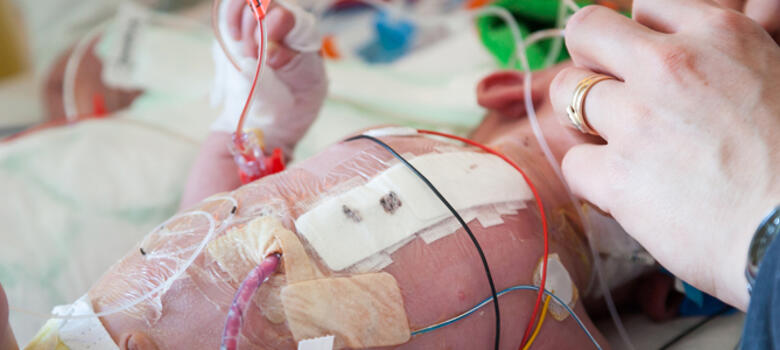
“There are a number of conditions in which children are born without a reliable source of blood flow to the lungs. They might have a valve that has failed to develop or that is severely narrowed” says Hill. “Historically, surgeons would insert a shunt made of durable fabric between the systemic and pulmonary arteries, but this is very high-risk surgery. Shunts are also unstable and prone to clotting off, which produces a life-threatening emergency.” These patients can now be treated with stents, which are inserted using a needle stick into an artery in the neck or leg. The stents are then tunneled through the vessels into a fetal vessel called a PDA. Ordinarily the PDA closes after birth but the stent is inflated across the vessel to hold it open. The stent procedure avoids neonatal surgery and the many complications associated with shunts, particularly for small infants who can sometimes weigh under 2 kg.
3 - Closure of PDA Occlusions in Extremely Premature Infants
In premature babies, the PDA sometimes stays open when it should be closed. In this situation the extra blood flow to the lungs can damage an infant’s lungs. This presents a challenging management scenario for high-risk infants, but Duke cardiologists have been able to close PDAs in premature infants who weigh less than 1,000 g. Hill explains that the procedure requires tunneling up from the femoral vein to insert plugs; the plugs block the vessel and stimulate scar tissue, resulting in a permanent repair to the heart. “We’re seeing significant improvements in these infants’ pulmonary status after the procedure, and it’s an approach we want to use more frequently, even in extremely premature infants who weigh as little as 700 g,” Hill says.
Advances at Duke
The catheterization lab’s director and pediatric cardiologist Gregory A. Fleming, MD, MSCI leads all of the innovations in the lab, and specializes in pediatric and adult congenital interventional cardiology. “We’ve made tremendous advances in the last decade in treating diseases that used to require open heart surgery; we can now treat these with a much less invasive approach in the cath lab,” he says. “We strive to stay on the forefront of new technology and have participated in numerous clinical trials which have been instrumental in getting new devices on the shelf for use in children and adults with congenital heart disease.
Fleming adds that Duke’s interventional and surgical teams collaborate to perform “hybrid” procedures. “This collaboration allows a less invasive approach to implanting devices that can only be implanted with a surgeon’s assistance,” he says.
“Managing complex congenital heart disease in children involves close collaboration among cardiologists, radiologists, surgeons, anesthesiologists, and intensive care unit physicians. Our program at Duke has had positive outcomes over the past several years, and our team is accomplishing incredible things by working together,” says Hill.
Joseph W. Turek, MD, PhD, chief of pediatric cardiac surgery at Duke, says the catheterization innovations are an indication of the Duke Pediatric & Congenital Heart Center’s dramatic growth and evolution. “We are becoming a major regional referral center because of our team’s ability to innovate, work together, and successfully help even the most complex pediatric heart presentations,” he says. “Importantly, our outcomes are second-to-none and we look forward to providing these services to children and their families across the Southeastern U.S.”