Duke Cancer Institute (DCI) is a leader in the multidisciplinary care of gastrointestinal (GI) cancers, including cancers of the colon and rectum, stomach, liver, pancreas, anus, gallbladder, and bile duct. Patients with GI cancers benefit from the team’s commitment to advancing treatments through novel medical therapies, adopting innovative surgical approaches, and expanding DCI’s GI cancer clinical trial portfolio.
“The magic of working at Duke is our multidisciplinary team. We have world-class specialists coming together to offer the very best treatment for each patient,” says Sabino Zani Jr., MD, hepatopancreatobiliary surgeon. He adds, “We personalize treatment plans to get the most optimal outcomes; there’s no one-size-fits-all approach.”
Through multidisciplinary tumor board meetings, Zani is one of up to 30 specialists reviewing all liver, pancreas, and biliary cancer cases. This includes experts from medical oncology, radiation oncology, radiology, gastroenterology, hepatology, surgery, and transplant, all contributing to developing an individualized care pathway.
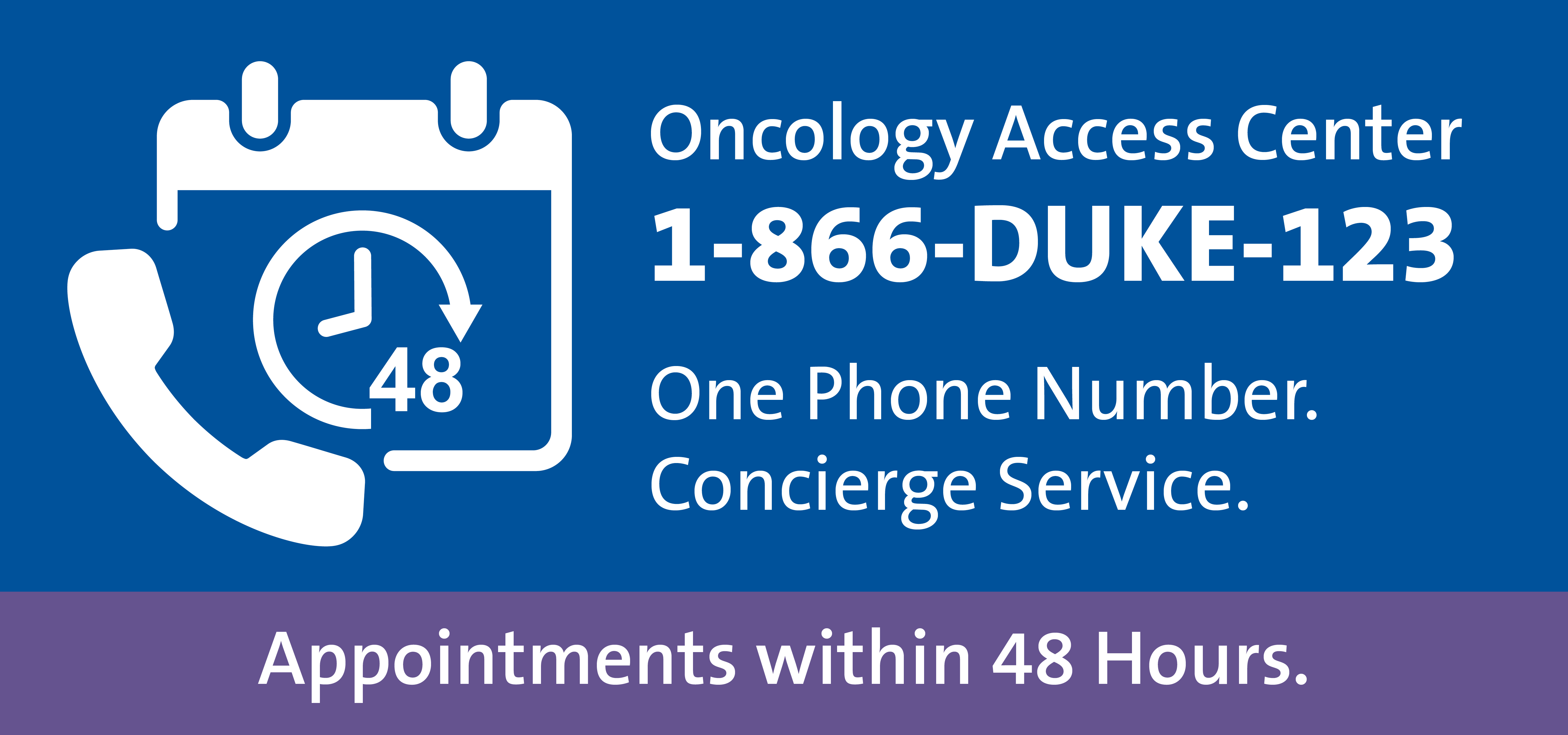
Call the referring provider team Monday through Friday between 8:00 a.m. and 4:30 p.m. at 866-385-3123 (1-866-DUKE-123). You can also email OncologyReferral@Duke.edu or fax 919-613-2316.
Robotic and minimally invasive surgery innovation
A distinguishing aspect of Duke is its commitment to advancing robotic and minimally invasive surgery, as well as translating novel approaches into clinical practice. As the co-director of the Duke Surgical Education and Activities (SEAL) Lab and the chair of the Duke Robotics Committee, Zani is actively leading surgical advancements and clinical training that improve direct patient care across the system.
“We’ve been building our robotics program at Duke for 15 years, and we’re expanding robotic applications and training more surgeons across the entire Duke Health system,” says Zani. Including all surgeries representing all specialties, Duke has performed over 4,000 robotic cases between July 1, 2024, and June 30, 2025, and projects a 10-15% growth in the year ahead.
Surgical procedures to treat GI cancers are complex and can have high risks. “Using minimally invasive techniques, we can achieve the same, if not better, surgical results but with a faster recovery time for patients compared to larger, open procedures,” explains Zani.
Quicker healing, return to life
According to Zani, when completed with modern minimally invasive techniques, operations to resect or treat GI cancers typically lead to a shorter hospital stay after surgery, a quicker return to baseline recovery, fewer surgical and post-surgical complications, and equal oncologic outcomes. These benefits are significant because any complications or morbidities can delay the next phase of care for patients, potentially impacting their outcomes.
Zani adds, “At Duke, we not only have world-class surgeons, but also specialists at the top of their fields in medical oncology, radiation oncology, immunotherapy, and other modalities of care after surgery.”
Pancreatic and liver cancer expertise
Pancreatic cancer is a challenging disease to treat. Historically, pancreatic cancer surgeries have had complication rates as high as 60%, which can slow recovery and limit the potential of receiving other modalities after surgery. “Our hepatopancreatobiliary surgeons are doing very complex Whipple procedures robotically, which has reduced post-operative length of hospital stays by one to two days compared to open procedures, while also reducing infections and complications,” says Zani.
For liver cancer resections, surgical procedures have historically been associated with larger incisions, potential complications, and prolonged hospital stays. Zani says that robotic approaches have changed that. Hepatic infusion pumps are also being placed through robotic techniques, delivering chemotherapeutic agents directly to the liver. “These used to be open procedures that we’re now successfully doing minimally invasively.”
Depending on the disease process, liver transplant can also be a potential path for patients. “At Duke, robotic approaches are also applied to hepatic resections for living donors, which helps donors recover quicker,” says Zani. Duke is one of the few centers in the country with protocols in place to perform liver transplants for colorectal cancer metastasis.
For referring physicians, Duke’s GI oncology team is available at DCI locations in Raleigh, Cary, and Durham for any level of support. “We’re happy to consult on cases, treatment planning, surgical options, and clinical trials to collaboratively develop a plan that’s best for each patient,” says Zani.
