Increase in Living Donors Accelerates Transplant Growth
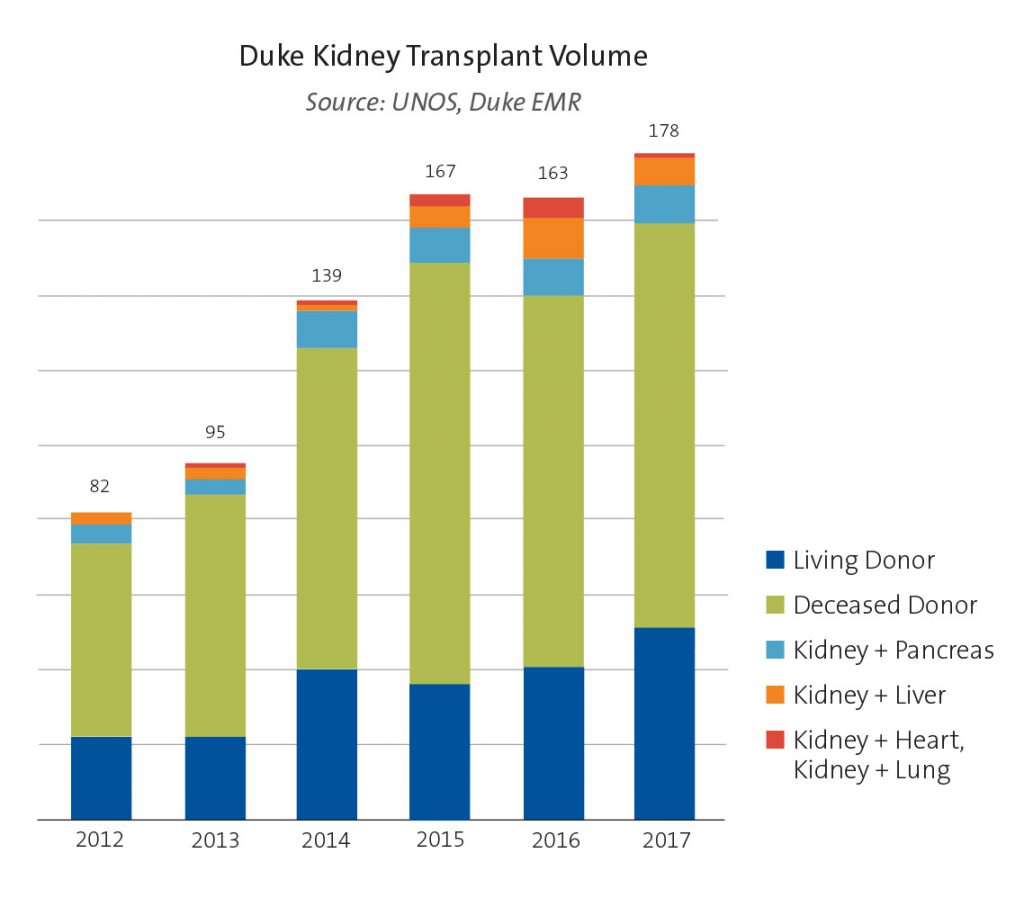 Figure. Duke kidney transplant volume, 2012 to 2017.
Figure. Duke kidney transplant volume, 2012 to 2017.
The Duke adult kidney transplant program continues a rapid growth trajectory—more than doubling the number of annual procedures since 2012—by bolstering its living donor program and accelerating referral responses and pre-transplant evaluations.
During 2017, 178 adult kidney transplants were performed at Duke; in 2012, the volume was 82 (see Figure). The growth is particularly significant because of a decline in kidney donations across the United States during those years.
“Many factors contribute to our success, but the fastest growing aspect now is the living donor program,” says Matthew J. Ellis, MD, medical director of the Adult Kidney Transplant Program. “By investing in the living donor program and making a daily commitment to the effort, we reduce wait times and ensure better organ quality.”
More than 30% of Duke kidney transplant patients receive their kidneys from living donors. Approximately 40 living donors were added during 2016, and the number of living donors has increased steadily since 2013.
“Patients are encouraged to use social media to solicit donors,” Ellis says. “About half of our living donors are related.” Other donors are “directed,” typically spouses or friends. Social media has attracted altruistic donors who want to help, Ellis says. But increasing donor totals is just a single element of the program’s success.
The team’s rapid response to patient inquiries and referrals accelerates patient assessments and shortens wait times. Following a referral, patients are offered evaluations within 3 days while most centers require 4 weeks. Rigorous post-transplant protocols help patients leave the hospital in 4 to 5 days with detailed medical direction.
“We have a coordinated approach to the entire process, from accelerating initial appointments to managing each step for new patients and ensuring that the patients can be discharged promptly,” Ellis says.
The discharge schedule depends on the patient’s condition, Ellis cautions, noting that creatinine management, bowel function, and other essential recovery metrics must be evident.
In addition to a long-term track record of successful outcomes, the program accepts increased-risk organs, including those from deceased donors with HIV, hepatitis C, or hepatitis B.
