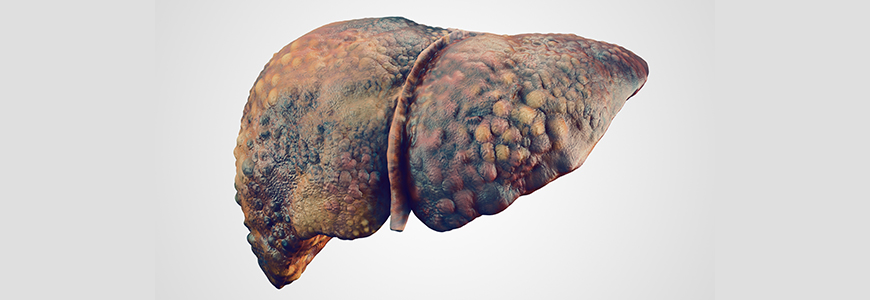
The incidence of severe alcohol-associated liver disease (ALD) including both acute alcoholic hepatitis (AH) and alcohol-associated cirrhosis has been rising in the United States, especially among younger people, particularly women.
The spike in ALD presentations—exacerbated by the COVID-19 pandemic—has triggered a national effort among liver transplant centers to integrate mental health counseling, addiction treatment, and alcohol cessation therapies into treatment for these life-threatening conditions.
Between 2017 to 2020, ALD mortality rates rose from 13.1 to 16.9% in males and 5.6 to 7.7.% among females. The surge of patients presenting with life-threatening ALD has required liver transplant programs to provide more integrated, collaborative resources to help patients maintain abstinence before and after transplant.
While many liver transplant centers previously required a period of abstinence—typically six months prior to proceeding with liver transplantation—specialists say data shows that liver transplantation can be performed safely in a select group of patients with acute alcoholic hepatitis without a period of abstinence prior to transplantation.
“The rising incidence of severe ALD has led to a national effort among transplant programs to create more standardized recommendations to assess candidates with alcoholic hepatitis for liver transplantation,” says Lindsay Y. King, MD, MPH, a transplant hepatologist and medical director for the Duke Liver Transplant Program.
To facilitate a solid organ transplant evaluation for your patient, please refer to our transplant referral forms.
Patients too sick to wait for six-month abstinence delay
Many patients who need a liver transplant are too sick to wait for a six-month period of abstinence, King says. Additionally, research has not demonstrated that waiting a specific number of days or months to demonstrate abstinence predicts future relapse risk.
This has led transplant teams to look at other variables associated with risk for post-transplant relapse including prior liver decompensation, previous treatment history and caregiver support. The transplant teams focus more on support systems, addiction, and mental health treatment after transplantation.
During a three-year period from January 2019 to January 2022, the Duke Liver Transplant program performed transplants for 69 patients with ALD, according to Stephanie Garbarino, MD, a Duke hepatologist and transplant specialist.
At Duke, a multidisciplinary team of social workers, psychologists, hepatologists and surgeons have worked to develop pathways to assess patients for candidacy for transplantation for alcohol-associated liver disease and connect them to addiction resources before and after transplantation. Garbarino leads research in predicting and assessing relapse risk following liver transplantation.
When patients present with acute alcoholic hepatitis and do not respond to traditional therapies, liver transplantation may be considered even when patients have not had a period of prolonged abstinence before transplantation, King says.
Ongoing addiction treatment and mental health support post transplantation, King adds, is required because there is no safe amount of alcohol use following transplantation.