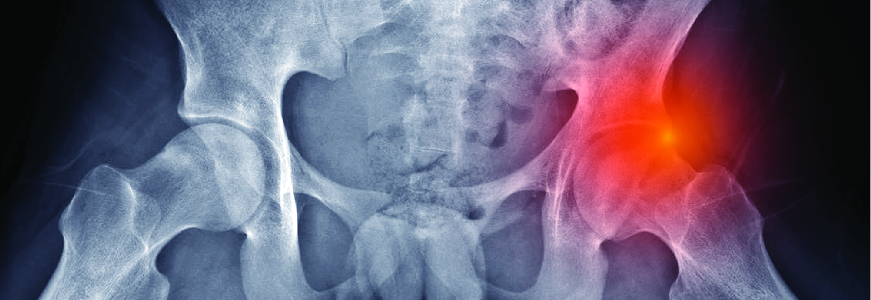
An emphasis on hip preservation for younger patients who present without arthritis guides the practice of Duke surgeons focusing on periacetabular osteotomy (PAO), femoroacetabular impingement (FAI), and arthroscopic procedures in a growing Duke clinic.
Brian D. Lewis, MD, chief of the Hip Preservation Section within Duke’s Department of Orthopaedic Surgery, says demand for PAO and FAI have increased steadily since 2015, as younger patients seek surgical solutions to painful hip dysplasia or impingement that limit their active lifestyles.
“Each patient will have a slightly different presentation, of course, but the conditions affect their ability to be active and function as fully as they want to,” Lewis says. “The pain may affect their mobility at home or even sitting in a work environment. For others, the pain may be most present when driving.”
FAI is the most commonly performed surgery within the Duke program and has increased approximately 50% in recent years, Lewis says. Requests for PAO are rising, too, and have doubled in the past decade.
“We have worked to position ourselves as leaders in diagnosis and treatment of nonarthritic hip conditions, and we’ve been able to build the program,” Lewis says. “We now have a wide referral network from across the Southeastern U.S.” Steven A. Olson, MD, and Richard C. Mather III, MD, MBA, work with Lewis in the clinic. All are hip specialists whose practices include arthroscopy and surgery. Olson is also trained as a trauma surgeon.
Evolving trends in hip preservation
The surgeons combine physical therapy with surgery, Lewis says. If a surgical option is chosen, the procedure is performed arthroscopically if possible. Treatments for non-arthritic hip dysplasia have continued to evolve, often involving both surgery and arthroscopy.
“The PAO we do now was developed in the mid-1980s,” Lewis says. “Now, we are working with much younger patients, and the procedure has evolved to be much more friendly to soft tissues. While tendons were removed from the bone in early versions, we now deploy tendon-sparing techniques to encourage earlier mobilization and quicker recovery.”
Another growing trend is the incorporation of arthroscopy into PAO to enable visual access to treat conditions that may exist within the joint, Lewis says. Hip arthroscopic treatments also continue to evolve, and FAI is now treated predominantly with arthroscopy, he adds. Occasionally, a patient with severe hip deformity or disease may require a surgical solution.
Factors related to increase in hip dysplasia cases
The reasons for the increase in patients presenting with conditions related to hip dysplasia are not clear, Lewis says. “Some of this is obviously caused by increased recognition within medicine. Awareness of dysplasia and its treatment options are more common in orthopaedic training programs.”
But Lewis says identification and medical training are not the primary factors in the increase. “We know that participation in sports by young people can increase the risk of hip dysplasia later in life,” he says. “Clearly, more people’s hips are growing in ways that create these conditions, but playing sports is probably just one reason we can identify.”
Orthopedic research has demonstrated that ancient skeletons do not display signs of hip dysplasia, Lewis says, an indication that the increase is probably the result of factors not yet fully understood.