A 69-year old female patient who had undergone five shoulder-related surgeries self-referred to the Duke Health orthopaedic team to request an assessment of her complex shoulder condition.
Although active and in generally good health, she was frustrated by the ineffectiveness of previous procedures that failed to resolve pain and inflammation associated with severe shoulder arthritis. Previous surgeries included a rotator cuff repair and shoulder replacement.
Despite the surgeries, she faced daunting physical challenges: she could only shrug her right shoulder, which remained useless and painful. Her right arm dangled from the shoulder joint, impossible to lift or control. The shoulder’s skeletal structure was no longer attached to muscle or connective tissue.
Of greater concern to Duke specialists, the shoulder replacement device implanted previously was at risk of puncturing her skin, a development that could result in a painful, difficult-to-treat wound, introducing a significant infection risk.
After evaluating her shoulder and considering treatment options, what recommendations did the Duke team offer this patient?
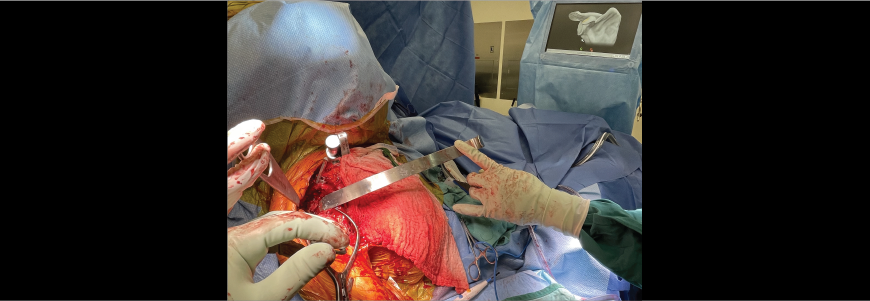
Oke A. Anakwenze, MD, MBA, a surgeon and head of Duke’s shoulder section, recognized the presentation from previous research. The patient needed a shoulder replacement but lacked enough muscle tissue to cover and connect the new implant. Anakwenze proposed a complex remedy that proved successful: The surgical team performed a flipped bipolar pectoralis transfer, which required assistance from a plastic surgeon experienced in soft tissue repair. Following the February procedure, the patient is recovering as expected.
Anakwenze and colleagues had researched surgical solutions for this condition before the patient contacted Duke. Although rare, the condition is familiar to experienced orthopaedic surgeons. Only a few medical centers in the United States have performed the pectoralis transfer; Duke is one of two centers in North Carolina who have completed the procedure.
“When we saw the patient and studied the challenges associated with her shoulder condition, our team knew we could offer a potential solution,” Anakwenze says. In addition to orthopaedic colleagues, Anakwenze sought the expertise of Suhail K. Mithani, MD, a plastic surgeon with extensive experience in repair and reconstruction of soft tissue, an essential part of the procedure.
After meeting with the patient and reviewing the physical challenges with the shoulder, Anakwenze practiced the surgical technique using a cadaver with Duke orthopaedic surgeons Yaw D. Boachie, MD, and Christopher S. Klifto, MD.
“We wanted to make sure we could anticipate any issues,” Anakwenze says. The procedure required releasing the pectoralis major from the clavicle as well as a two-third release from the sternum, Anakwenze says. The pectoralis was then flipped for reattachment.
“This patient had lost a lot of her soft tissue coverage within the shoulder as well as about a third of the deltoid,” Anakwenze says. “That was the reason the implants were about to come through her skin. Because of long-term inflammation from arthritis and the outcomes from previous procedures, she essentially had a useless upper right torso that involved the shoulder and arm.”
The procedure accomplished two objectives, Anakwenze says. First, it offered renewed shoulder function by using the pectoral muscle instead of the deltoid. The pectoralis muscle is flipped and placed where the deltoid had been previously. Second, it restored function in her arm by offering new muscular options. The surgical team also worked with the plastic surgeon to preserve and maintain the neurovascular pedicle.
“This is a pretty rare procedure,” he says. “First, it’s very challenging to perform and it involves significant risk. It is a good solution for the patient who is truly indicated for this procedure. But these patients are not seen commonly.”
Duke’s multidisciplinary approach offers the best option for patients facing complex challenges, particularly for rare presentations, Anakwenze says. The patient’s pain is negligible and functional use of her arm and shoulder is improving.
“This is not a surgery we undertake to help a patient return to an active, sports-focused condition,” he says. “But given her surgical history and challenges with arthritis, she should have a high level of function that she lacked previously.”