Since performing the first deep brain stimulation (DBS) procedure for epilepsy in North Carolina in 2019, neurosurgeon Derek Southwell, MD, PhD, has treated nearly 30 patients and is working to advance Duke’s armamentarium of innovative treatment options for drug-resistant epilepsy and movement disorders.
After DBS, most but not all patients will experience a great improvement in quality of life, with an average reduction in seizure frequency of approximately 70%. Still, physicians and patients are often unaware of this surgical option for epilepsy, Southwell notes.
“DBS can be applied in cases where it’s difficult to fully identify where seizures originate,” says Southwell, the surgical director of the Duke Comprehensive Epilepsy Center. “It is also a valuable option in cases where the seizure onset areas are known, but they happen to be multiple, or too large, or too vital for function to remove.”
Awake vs. Asleep DBS
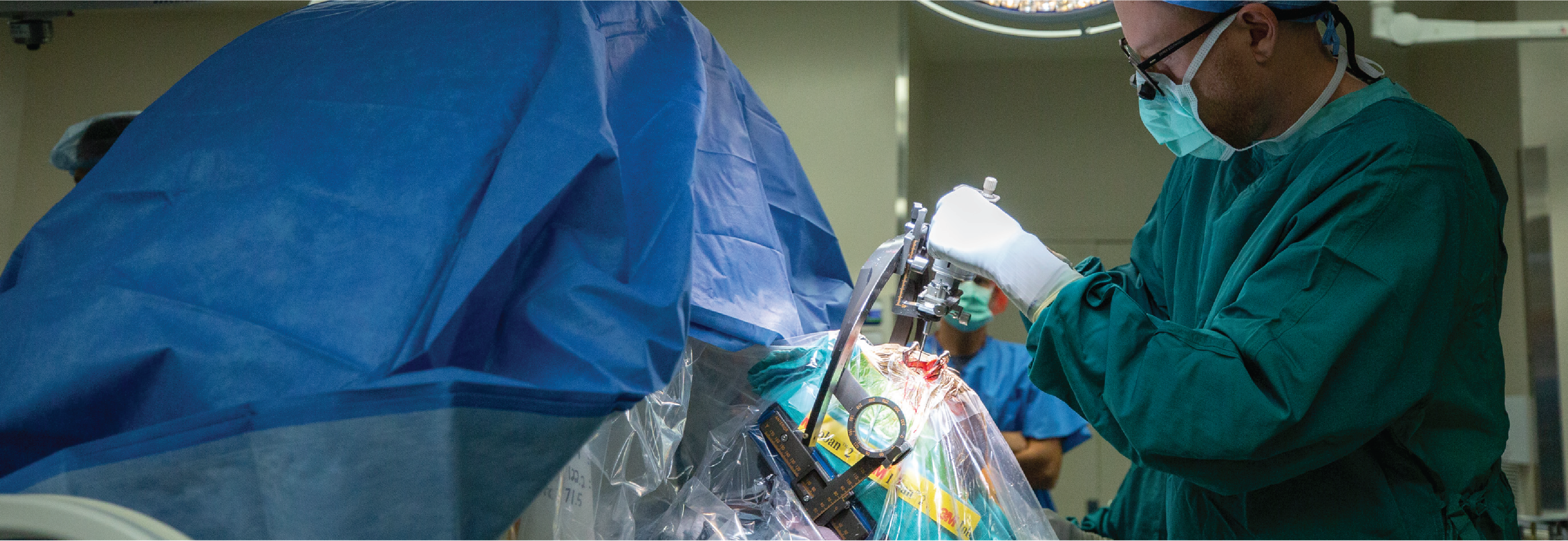
DBS surgery, although a newer treatment for epilepsy, has been used to treat movement disorders for more than 20 years. Traditionally, DBS for movement disorders has been performed while the patient is awake, but newer techniques using interventional MRI allow precise placement of DBS electrodes while the patient is asleep. Notably, Southwell has performed essentially all of the interventional MRI DBS placements in North Carolina.
For some patients, this newer asleep DBS procedure can increase the comfort and safety of DBS surgery. Overall, it allows surgeons like Southwell to provide DBS to a broader range of patients.
Interneuron Transplantation Research
In addition to his clinical practice at Duke, Southwell is exploring how the transplantation of interneurons — brain cells that provide inhibitory signals to partner brain cells — can be made safe and effective as a therapy for epilepsy.
Southwell and others have shown that interneurons can be transplanted into the rodent brain, where they modify the neural circuits of the recipient. Grafting new inhibitory interneurons into the recipient brain can reduce the activity patterns that give rise to seizures. If successful in humans, this therapeutic approach has the potential to reduce epileptic seizures with less surgical invasiveness, risk, and impact on brain function.
This technology has potential implications beyond epilepsy, says Allan Friedman, MD, Duke Neurosurgery chair. “Dr. Southwell’s work has so much potential to restore function to patients who have lost function secondary to stroke, trauma, or neurological diseases,” he adds.
Advancing DBS Programming, Clinical Education Opportunities
Cameron McIntyre, PhD, recently joined the team of neural engineers and scientists at Duke working to advance the existing technologies behind DBS. A biomedical engineer with more than 20 years of research experience in neuromodulation, McIntyre has already developed numerous DBS technologies and is focused on solutions for improving the placement accuracy of the implanted electrodes.
“I'm really interested in working on how to bring together the best preoperative MRI data, with the best surgical planning models, to the next generation of neurosurgical robots,” he says. The research projects involve using reverse-engineering to refine the existing DBS software for the robotic stereotactic assistance device used in DBS surgery. “This work has the potential to improve DBS electrode placement and programming and help clinicians optimize the therapy for each patient,” he says.
McIntyre is also working on developing holographic clinical education materials for the DBS community, which would enable participants to visualize and interact with the models. “There is a substantial appetite for scientific education content around DBS,” he says. “This would be a powerful tool to help clinicians around the world understand the fundamental biophysics of how these devices actually work in the brain.”
With so many resources dedicated to improving DBS placement, targeting, and programming, the Duke team is keen on making technological advances that can rapidly reach clinical applications. “It’s not common to have so many neurosurgery, neurology, and engineering collaborators working together at one institution, and we are all striving to get new technologies into clinical practice in our lifetime,” says McIntyre.