Benefits of Partial Heart Transplants
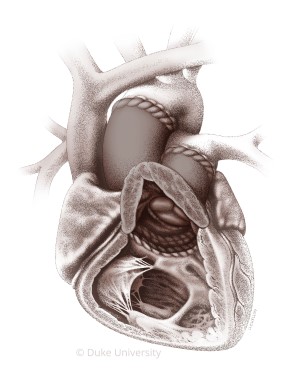
New research shared in the Journal of the American Medical Association validates partial heart transplant, showing that the new manner of valve procurement used during the partial heart transplant led to two well-functioning valves and arteries that grow in concert with the child as if they were native vessels.
In addition to extending the donor pool, partial heart procedures reduce the need for whole heart transplants and multiple surgeries. Other solutions, such as deceased donor grafts and mechanical valves, require replacement as the child grows.
“Children have to have valves that are going to grow with them,” Turek says. “These children who would normally need multiple operations in their lifetime could potentially be one-and-done with the partial transplant.”
Using a single procedure reduces the risks associated with every open-heart surgery. Living organs have also shown better results and survival rates than deceased donor. In addition, partial heart recipients have received about a quarter of the amount of immunosuppressant medication as a full heart transplant, reducing the potential for subsequent organ damage. “What we’ve found after doing several of these is that the dose required is usually non-life altering,” Turek says.
To facilitate a solid organ transplant evaluation for your patient, please refer to our transplant referral forms.
Partial heart transplants have also successfully treated patients with truncus arteriosus. Turek is currently working in the lab to test the procedure as a treatment for other cardiac valve insufficiencies. “Any kind of valve pathology, we can leverage the partial heart transplant to help that diseased state. Children who need pulmonary or aortic valves or with different presentations of tetralogy of Fallot can also benefit from the procedure,” Turek says.
As a clinical leader, Duke has performed more than two-thirds of all partial heart transplants in the world since pioneering the procedure in 2022. Recognized by U.S. News & World Report as the #2 hospital for pediatric heart care in the nation, Duke performs over 400 life-saving congenital heart surgeries annually, with shorter wait times and better survival rates for heart transplants than the national average.
The Duke team continues to evolve to handle more challenging cases, recently welcoming J. Brian Clark, MD, who specializes in surgery for pediatric and congenital disorders. Clark joins the team as executive co-director of the Duke Pediatric and Congenital Heart Center.