When a 26-year-old woman with cystic fibrosis began to reject her second set of transplanted lungs, she was left with few options. The centers where she’d received her previous transplants couldn’t perform the procedure for a third time. With her lung capacity dwindling, the patient was referred to Duke’s lung transplant program for a “three-do” procedure.
A repeat transplant is a difficult undertaking. Each procedure leaves scar tissue, and subsequent procedures must deal with the results of previous surgeries, including adhesions. “Vital structures like the pulmonary arteries, pulmonary veins, and airways, which are right next to one another, can become fused together in transplant surgery,” says Matthew G. Hartwig, MD, lung transplant surgeon and surgical director of the Duke Lung Transplant Program. “It can become difficult in later procedures to separate those structures. Every time you do it, it gets a little bit harder.”

To facilitate a solid organ transplant evaluation for your patient, please refer to our transplant referral forms.
Comprehensive lung transplant care
To be eligible for a repeat transplant at Duke, patients must meet criteria including age, overall health, other vital organs strength, functional status, nutritional health, and access to appropriate care in their community. Once a patient has been identified as a good candidate, they must travel to Duke for an extensive “prehabilitation” program for physical conditioning and education to improve their functional status before surgery.
“Our nurse coordinators and other team members meet with patients to help with breathing techniques, speech therapy, pulmonary rehab, nutrition, and more,” says John M. Reynolds, MD, transplant pulmonologist and medical director of the Duke Lung Transplant Program. “The support continues through their time in the hospital and after.”
The “three-do” patient arrived in Durham in the fall of 2023 to prepare for her surgery in January 2024. The surgery was successful, with only one postoperative subpleural hematoma that required a takeback. Now home again, the patient is regaining her strength and has shown no signs of rejection.
The Duke lung transplant program
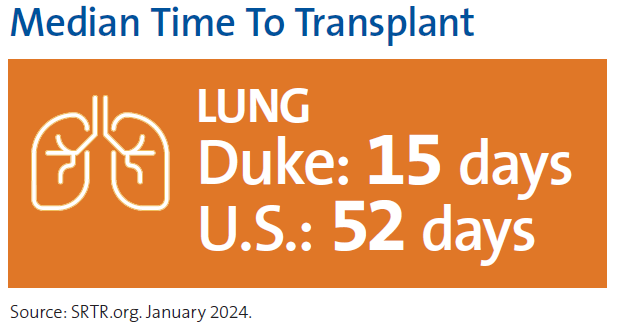
Duke continues to lead the field of lung transplant, with a median wait time of 15 days, the shortest in the U.S., compared to a national average of 58 days. With more than 2,500 total procedures, they have performed the most lung transplants in the country. Duke physicians also help to advance the field through clinical trials. Current studies include trials to test drugs to help prevent inflammation, lung injury, rejection, and chronic lung allograft dysfunction.
Duke’s experienced, multidisciplinary team is able to address even very complex cases. “Surgeons, pulmonologists, nurse coordinators, nutritionists, financial coordinators, psychologists, and social workers meet weekly to review transplant referrals,” Reynolds says. “We discuss and receive everyone’s collective input as to whether candidates are suitable for transplant or if they have modifiable conditions that could make them acceptable.”
With this procedure, Duke has performed 13 of the 23 third or more repeat lung transplants in the country based on data from the Organ Procurement & Transplantation Network (OPTN). This experience and expertise allow Duke to take on cases that other centers may not be able to handle. “With expanding guidelines, anyone with end-stage lung disease without medical options should be referred to give our transplant team the opportunity to assess those patients,” says Hartwig.
Reynolds agrees: “We’re always happy to review records to see if we can help someone who has been rejected elsewhere.”