Heart failure (HF) is a serious disease that carries a high mortality risk: 50% of patients with HF die within five years. If a patient’s cardiac output falls too low, they are at risk of cardiogenic shock (CS), a diagnosis that rose threefold in the U.S from 2004 to 2018. “There’s no prescribed pathway to treat patients in cardiogenic shock,” says M. Imran Aslam, MD, an advanced HF specialist and interventional cardiologist at Duke Health. “Caring for these patients is an art.”
Aslam’s training — including dual fellowships in advanced HF and interventional cardiology — brings unique expertise to Duke Heart. “Training in both interventional cardiology and advanced heart failure is becoming more common, providing the most critically ill patients with options for both revascularization and advanced heart failure therapies,” says interventional cardiologist W. Schuyler Jones, MD, Duke’s director of Invasive Services and the Cardiac Catheterization Laboratories, which treats patients with CS. “Often, these patients have no other chances for survival, and now we’re able to give them opportunities.”
CS and mechanical circulatory support
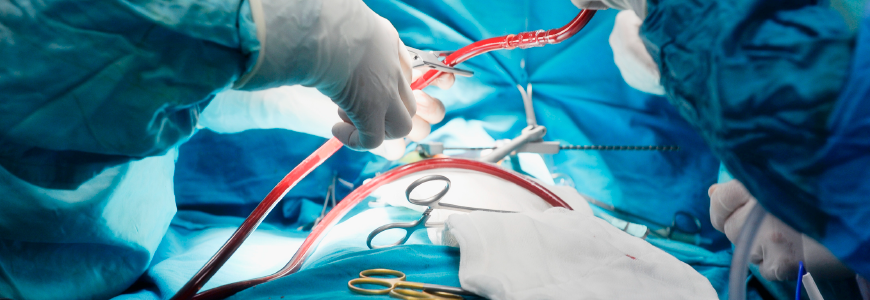
CS can be difficult to diagnose. In addition to the classic signs of low blood pressure and weak or erratic pulse, CS may present with confusion, syncope, fever, or kidney or liver dysfunction. The first-line treatment for all complex coronary disease is guideline-directed medical therapy (GDMT) and pursuit of coronary artery revascularization. However, if GDMT fails, surgery and/or mechanical circulatory support (MCS) may be indicated.
“When the heart can’t supply the brain and other organs, mechanical support like ECMO [extracorporeal membrane oxygenation] can be required,” says Aslam. ECMO is usually used to facilitate surgery, but it can also support a patient in CS to prepare for a transplant or ventricular assist device (VAD). An interventional cardiologist on the ECMO team uniquely positions Duke to provide advanced care.
Adding to treatment options
In addition to ECMO, VADs are also a form of MCS. “Many times, an LVAD [left VAD] will be sufficient, but when it isn’t, we give the right side of the heart temporary support through minimally invasive heart pumps and temporary right VADs to nurse the heart through the insult of surgery,” Aslam says. “Other patients may need a total artificial heart, which our amazing surgical team is able to implant.”
With a broad range of treatment capabilities, Duke can offer more options to critically ill patients. Duke led the country in advanced HF volumes in 2024, with 88 durable VADs and 132 heart transplants, offering the expertise to care for all stages of HF.
Aslam says, “We offer intermediate steps that are unique in the Triangle or even the state, especially for patients who may not be a candidate for LVAD and transplant but still need aggressive measures.” These options can include clinical trials, including those by advanced HF specialist Marat Fudim, MD, MHS, director of the Duke Heart Center Clinical Research Unit. “Especially for ischemic patients who’ve been turned down for revascularization or told there’s nothing more to do, think of us,” Aslam continues. “That’s not the final word. Always refer.”