In November 2018, the Duke Cancer Institute Melanoma Program in partnership with the Preston Robert Tisch Brain Tumor Center launched a phase 1 clinical trial assessing the safety of the genetically recombinant, nonpathogenic poliovirus/rhinovirus chimera PVSRIPO in patients with advanced melanoma. The study follows exciting results from a recent phase 1 clinical trial that showed that patients with recurrent WHO grade IV malignant glioma had improved survival following treatment with the therapy.
Although PVSRIPO has never been tested in patients with melanoma, there are good reasons to think the therapy may be effective for these patients as well, says the study’s principal investigator, surgical oncologist Georgia Beasley, MD, MHSc. Among them: Malignant glioma and melanoma both express the receptor for poliovirus. There are also preclinical data from the labs of Duke neurosurgery professors Smita Nair, PhD and Matthias Gromeier’s, MD, supporting the use of PVSRIPO for melanoma treatment.
The Duke trial is enrolling nine patients with unresectable, recurrent stage IIIB, IIIC, or IV melanoma, divided into three dosing cohorts receiving one, two, or three injections of the treatment. Patients must have at least one injectable lesion and have failed at least one anti-PD-1–based therapy. Patients with BRAF mutations must have failed at least two lines of therapy.
The trial’s primary outcome measure is the proportion of patients with dose-limiting toxicity in each cohort after two years. Secondarily, biopsies will also be taken both before and after treatment for immunologic analyses.
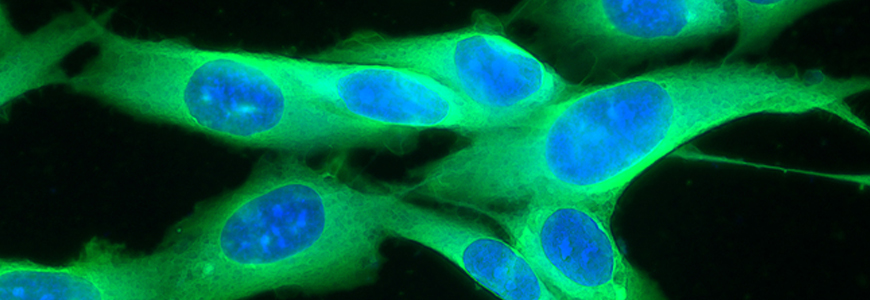
The biopsies will be a valuable tool to assess each patient’s immune response to the treatment, Beasley says. The research team, which, in addition to Beasley, Gromeier, and Nair, will include professor of surgery Eda Holl, PhD, and postdoctoral fellow Mike Brown, PhD, will measure CD8+ T-cell recruitment as well as evidence of inflammation, among other changes to the tumor microenvironment following PVSRIPO treatment.
Beasley is hopeful about the potential impact of the trial. Although there have been major advances in the treatment of advanced melanoma, particularly with the introduction of PD-1, as many as 60 percent of patients do not respond to therapy and an additional subset of patients experience recurrence of their disease.
“There are still a lot of patients who we don’t have an effective treatment for,” she explains. “I think this therapy has the potential to either assist in making these patients more sensitive to PD-1 therapy or, by itself, have a direct treatment effect.”