To refer a patient to Duke Neurosurgery, call 919-684-7777.
A 44-year-old female patient came to Anoop Patel, MD, Duke neurosurgeon, after being diagnosed with a meningioma brain tumor. The patient presented to an ED in South Carolina after experiencing a seizure.
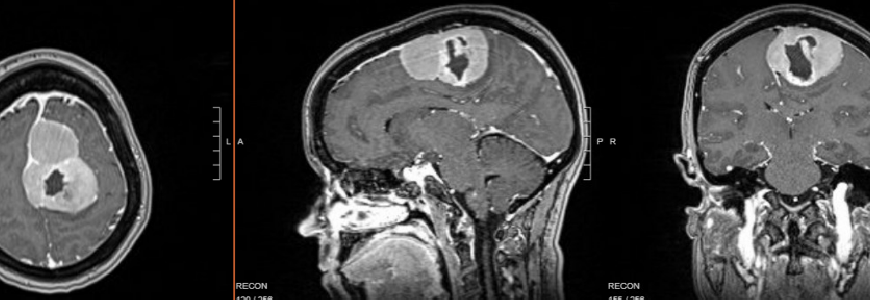
An MRI completed in the ER revealed a 6.9 cm by 5.0 cm by 4.4 cm meningioma in the anterior-posterior direction. She had experienced decreased motor function on her right side, a persistent headache, and a tonic contraction of the foot and leg tightening for several weeks leading up to the seizure.
The patient was then transferred to Duke for further evaluation. “The mass was in the parasagittal region of the brain, and it was directly compressing on the part of the brain controlling right leg movement,” says Patel.
Patel continues, “Resecting tumors in this location is challenging because they can contact the motor cortex. We also had to consider maintaining the integrity of the sagittal sinus and the collateral cortical veins. Interrupting the venous flow can cause severe swelling in the brain and is potentially life-threatening.”
Question: To ensure optimal outcomes for this patient, how did Patel approach the surgical plan?
Answer: First, advanced imaging was completed to visualize the patient’s tumor and its sensitive location. “The location of the meningioma made this a higher-risk procedure,” says Patel. “At Duke, we have advanced technology and refined surgical techniques. We also treat a high volume of meningioma cases, so we have the expertise and resources to maximize resections while minimizing complications.”
During the procedure, Patel utilized advanced imaging to monitor the venous structure and blood flow in the sagittal sinus. “We have a variety of technologies, like intraoperative Doppler, to guide our technique and protect the blood vessels.” Part of the tumor was touching a vein, but Patel was able to successfully remove the entire tumor, despite the complexity of its placement.
The patient recovered well, returned home to South Carolina, and resumed her active lifestyle rather quickly.
For meningiomas, “The first surgery is the best shot at a cure,” says Patel. “If you don’t get the best possible resection in the first surgery, the tumor can grow back more aggressively, patients can develop scar tissue, and this complicates long-term outcomes as well as response to additional modalities, like radiation, if that’s part of the treatment plan.”
Duke treats a high volume of meningioma cases, performing hundreds of meningioma resections annually, which elevates an expert level of subspecialty care and dramatically improves outcomes for patients. Patel explains, “Duke’s other subspecialists support patients who need continued care after surgery, with neurooncologists, radiation oncologists, and even cutting-edge tumor molecular sequencing to deliver a personalized care pathway for each patient.”