A new 3D surgical planning platform—the first in North Carolina and one of only a few in the United States—enables Duke spine surgeons to more quickly and precisely assess musculoskeletal alignment while significantly minimizing radiation exposure for adult patients.
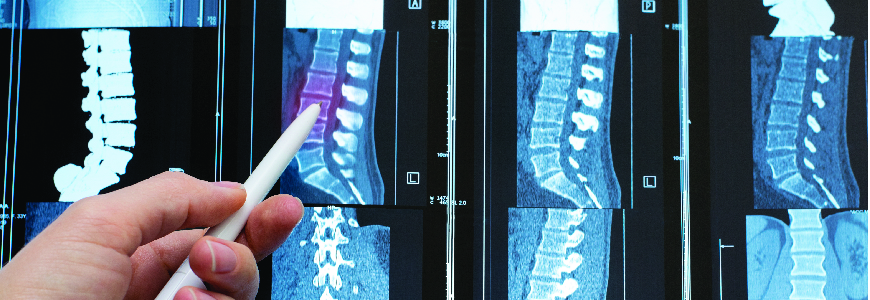
Traditionally, a surgeon combines multiple preoperative images to assess a patient’s spinal alignment and leg positioning. However, this advanced radiographic technology captures two full-body, weight-bearing images in less than 20 seconds with a radiation dose 50 times lower than conventional radiology, providing an accurate view of a patient’s spine and lower body in a natural standing position.
Since 2016, Duke has used the EOS system (EOS Imaging: Paris, France) for low-dose radiation spinal imaging, primarily with pediatric patients. The new system, EOSedge, was designed to provide better access to spine care imaging for adults, including those with high BMIs, and improve image quality. Duke spine surgeons can rotate and adjust the 3D parameters of the EOSedge images to better understand a patient’s spinal alignment in different positions and to optimize their pre- and post-surgical care plans.
Christopher I. Shaffrey, MD, chief of the Division of Spinal Surgery at Duke, says the ability to turn full-body imaging into 3D modeling improves the assessment of a patient’s spine alignment because it factors in the compensatory mechanisms that exist in the knees and hips.
“Achievement of alignment objectives has been shown to be the greatest predictor of successful long-term clinical outcomes,” Shaffrey says. “By having a better understanding of what the alignment should be, we’re able to personalize the specific correction and optimize care for patients with scoliosis, kyphosis, spina bifida, or other spinal pathologies that require revision surgery.”
Shaffrey notes that in addition to being used for spine care, this tool will serve as a long-term research platform for hip and knee replacement outcomes. In the future, it will also be used to optimize robotic-assisted surgeries, enabling smaller incisions due to the accuracy of preoperative planning.
“Our ability to better assess and inform the surgery with this technology helps us to best achieve and improve alignment and reduce complications for our patients,” Shaffrey says.