Since his arrival at Duke in January 2022, David M. Hasan, MD, MSc, has been working to push forward the research and tools available to help the 3% to 5% of the U.S. population who do not yet know they have had an aneurysm, which can lead to serious complications if it is not carefully surveilled.
“For patients with an unruptured aneurysm, they’re thinking, ‘Is this a ticking time bomb in my head? When do I treat it? How fast should I treat it? Do I need to change my activities?” he says. “All these questions create a lot of an anxiety for them, but it’s important to not simply jump in and treat an aneurysm.”
Treating an unruptured aneurysm requires expertise in differentiating stable from unstable aneurysms, and the risk of rupture is variable. “People used to think only large aneurysms or certain locations ruptured, but we now know that other factors contribute to the aneurysm formation and rupture, and we must treat each patient and every aneurysm as an individual,” Hasan explains.
Duke specialists like Hasan can help patients evaluate their treatment options and risk factors to determine what course of action is best for them. Dr. Hasan has treated more than 2,500 brain aneurysms using innovative techniques including awake surgery.
To refer a patient, log in to Duke MedLink or call 800-633-3853.
Unique Research Tools
“At Duke, not only are we very advanced in the surgical management of brain aneurysm, but we are also using unique research tools that help us understand more about the disease and help patients make more educated decisions about which option to do,” says Hasan.
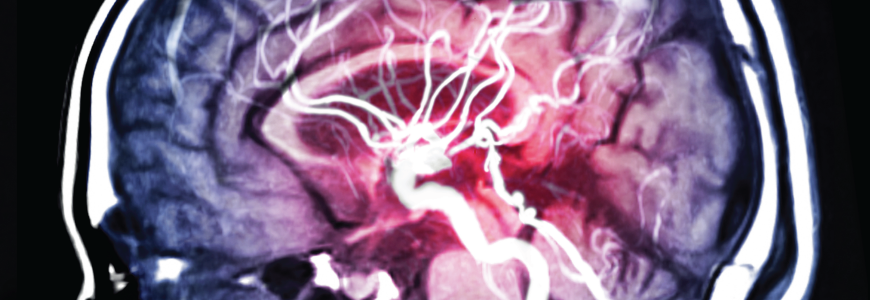
Below are a few highlights about Hasan’s research on imaging tools that help differentiate, study, and treat unruptured aneurysms. All these tools are being used and validated in small populations of patients, Hasan says.
Ferumoxytol molecular imaging. This technique uses a nanoparticle contrast to look for macrophages to indicate whether the aneurysm is inflammable, which would indicate a higher risk for rupture. Hasan was one of the first microvascular surgeons to work on this research in 2009.
The technique can only be used in select patients, Hasan cautions. Because of the possibility of severe side effects, the FDA issued a black box warning on its use for aneurysm, though it is approved for use in people with chronic anemia.
High-resolution vessel wall imaging. This approach uses traditional contrast (gadolinium) to predict which aneurysms are stable or unstable on MRI. “When we cannot suppress the signal of the contrast from white to black at the interface, there's residual contrast, which tells us that the aneurysm is slightly active in terms of changes,” Hasan says. “If we don't see anything, that gives us a signal that this aneurysm is stable and with those patients we recommend sometimes watching, especially smaller aneurysms.”
While it is associated with fewer side effects than ferumoxytol, it is generally a less reliable imaging tool.
Quantitative susceptibility mapping (QSM). With this tool, neurosurgeons are able to use the imaging sequence to quantify and detect a microbleed that cannot be seen from the surface of the brain. Because patients often present with what appears to be a migraine or tension headache, this tool helps Duke clinicians differentiate between people who may have a headache and those who may have an unstable aneurysm.
“If we see a microbleed in the QSM, we admit the patient immediately and treat them. That's when you know that the aneurysm is going to rupture imminently,” he says.