Treating a Large Pituitary Tumor
After noticing progressive bilateral visual loss and experiencing daily headaches for several months, a woman consulted an ophthalmologist, who recognized the signs of a pituitary tumor and referred the patient to the Multidisciplinary Pituitary Tumor Clinic at Duke.
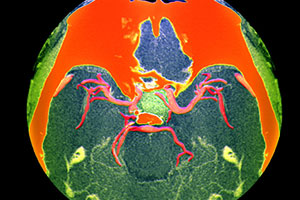
Imaging revealed a large pituitary macroadenoma 2.8 × 2 cm in size that extended outside the sella. Her optic nerve was also compressed.
Question: How did specialists at the clinic manage her condition?
Prior to performing surgery, it was critical to assess whether the tumor was functional and would first need to be medically managed. If, for example, the tumor is causing a deficiency in cortisol, Gratian explains, this needs to be treated prior to surgery to prevent serious illness or death during surgery. The evaluation is also important, she says, because some tumors do not require treatment or they can be treated by medical intervention alone.
The pituitary tumor was found to be nonfunctional and the patient had no clinically significant hormone imbalances, so the team opted to surgically remove the tumor.
“My expertise is in endoscopic and minimally invasive cranial surgery, and Dr Jang is an expert in sinus, nasal, and skull-base surgery,” says Codd. “By teaming up and working closely together in the operating room, we can remove large and complex tumors in a minimally invasive way.”
The surgery went well, and the tumor was removed with no complications. The patient’s headaches and vision problems resolved, and repeat magnetic resonance imaging 3 months after surgery showed no evidence of residual tumor. Her hormone levels immediately following the surgery and at her 6-week follow-up visit were also normal.
“A tumor this large can be challenging to remove without damaging the pituitary gland, and it can also reoccur,” Gratian notes. “That’s why it’s so important to also monitor postoperative hormone levels long-term.”
Gratian and Codd agree that being able to work closely together, in addition to enlisting Jang’s aid when necessary, is important for treating all their patients. “Dr Codd and I see patients together in our joint clinic,” Gratian says. “That way it’s easy to develop a plan for each patient and determine whether we need to bring in Dr Jang.”
Codd agrees: “It’s our continuity of care that’s so important and allows us to handle even the most challenging tumors.”