Using stem cells for in vitro research, a Duke biomedical engineer is advancing the development of precision medicine customized to treat diseases of the kidney.
By using novel applications of induced pluripotent cells (iPSCs) in kidney research, Samira Musah, PhD, is working to replicate the ways in which molecular signals and biophysical forces guide organ development and physiology.
Her kidney-focused research, Musah says, is driven by what she describes as “an escalating medical crisis in nephrology” as a growing number of patients suffer from kidney disease (KD) that often progresses to organ failure. Musah’s work is part of the MEDx initiative, a collaboration between the Duke School of Medicine and the Pratt School of Engineering, to inspire scientific innovation and develop new health technologies. MEDx was launched in 2015.
“My lab is motivated by the fact that more than 10% of the global population suffer from KD,” she says. “There are no targeted therapeutics associated with prevention; the drug pipeline is limited. Nearly 14% of the United States population suffer from kidney disease, and these patients can progress to end-stage renal disease. That leaves dialysis and organ transplantation as treatment options, neither of which is necessarily good.”
The lab’s focus on iPSCs is based on several key characteristics of the cells:
- iPSCs are important for the field of regenerative medicine because they can be propagated in culture indefinitely, offering an unlimited supply of stem cells. Researchers can minimize or completely avoid the need for multiple blood draws or more invasive procedures to derive cellular tissue from patients.
- iPSCs serve as a source of cells to replace human cells that are lost to injury or disease, as they can be directed to differentiate into almost any cell types in the presence of appropriate biochemical and biophysical cues.
- iPSCs can be engineered to simulate the function of many organs, mimicking functional processes and yielding results that are directly related to an individual patient’s biology.
Chemical and Mechanical Signals Differentiate Human Stem Cells
 Before the use of iPSCs, the lack of an effective system to study human kidney biology hampered therapeutic development, Musah says. Substantial differences between human and animal kidneys have stymied practical research. Many drugs deemed safe in animal tests failed in human applications due to toxicity that resulted in kidney damage.
Before the use of iPSCs, the lack of an effective system to study human kidney biology hampered therapeutic development, Musah says. Substantial differences between human and animal kidneys have stymied practical research. Many drugs deemed safe in animal tests failed in human applications due to toxicity that resulted in kidney damage.
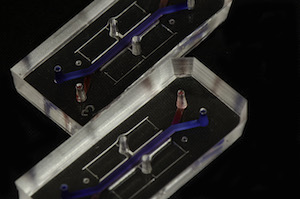
Musah’s lab uses chemical and mechanical signals to direct human stem cells to differentiate into functional kidney cell types. The lab extends their strategy to engineer complex multicellular systems including organoids and microfluidic organ-on-a-chip devices that simulates the kidney’s tissue patterning, blood flow, and molecular filtration processes.
The team created compartments within a microfluidic device to mimic the cellular structure, vasculature, and urine-creation characteristics of the human kidney. “The complexity of this system makes the data very rich and gives us insights we could not otherwise obtain using traditional tissue culture methods,” Musah says. “There are no other in vitro models that are able to mimic key features of human kidney development and function with specificity and efficiency.”
The stem cell-derived micro physiological systems allow the team to conduct experiments on the effects of specific drugs or treatment option on individual patients. “We can study disease phenotypes and inter-organ communication and do it all outside of the human body,” Musah says. Clinical application for patients may take several more years, she notes.
