Splanchnic nerve blockage (SNB) reduced both resting and exercise-induced pulmonary arterial wedge pressure in a follow-up study analyzing the effects of the nerve blockade on patients with heart failure (HF).
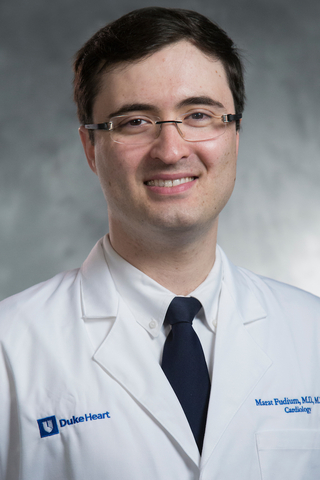
Published in June in the Journal of the American College of Cardiology: Heart Failure, the findings may offer a novel therapy for HF treatment, says Marat Fudim, MD, a Duke cardiologist and advanced heart failure specialist.
Fudim lead a previous first-in-human, proof-of-concept study, published in 2018 by Circulation and the European Heart Journal, analyzing the nerve blockage intervention in eleven patients with acute HF at Duke University Hospital. Fudim was one of a team of Duke cardiologists and researchers participating in both studies. The second was a prospective, open-label, single-arm interventional analysis in 15 patients with chronic HF who underwent SNB.
“This concept of using the nerve blockade in this way has the potential to shift our HF treatment paradigm,” says Fudim. “The bigger picture becomes evident when we look at the findings as a sequence of data coming together.”
The traditional treatment of fluid overload in patients with congestive heart failure involves the use of diuretics. In some cases, ultrafiltration is required to bypass the kidneys and filter water and salt from the body.
Heart, vasculature congestion not always driven by fluid overload
Congestion of the heart and vessels has long been identified as a symptom of HF, and requires a clinic visit or hospitalization to resolve, Fudim says. More recent evidence supports that congestion of heart and vasculature is not always driven by fluid overload or retention.
“Our current results challenge our long-standing dogma about the causes of and treatments for heart failure,” Fudim says. “Internal heart pressures are rising well before the fluid buildup and should become a significant marker.” This suggests that redistribution of internal blood volume might be as important as fluid retention.
The 15 HF patients underwent a temporary, medication induced SNB and then completed two exercises before and after the block. Following the SNB, researchers found lower intracardiac pressures. The hearts circulated more blood volume, and patients could exercise more rigorously. Stiffer heart muscle and vasculature makes it susceptible to develop elevated filling pressures with little addition of fluid or redistribution of blood in the body. During exercise, this fluid moves to the chest, triggering lung pressure that triggers dyspnea, limiting movement and exercise.
When the splanchnic nerve is blocked, fluid shifts to the belly, Fudim says, lowering pressure in the chest and the heart. Blockade of the nerve has also been used outside of the field of HF for the treatment of cancer-related pain.
“The significant pressure drop that occurs when fluid shifts away from the heart presents a new therapeutic opportunity,” he says.
This study was supported by the Translating Duke Health Initiative. Additional Duke collaborators include Adam DeVore, MD, MHS; Joseph G. Rogers, MD; Sunil V. Rao, MD; David Kong, MD; W. Schuyler Jones, MD; Cynthia L. Green, PhD; Michael Felker, MD; Adrian H. Hernandez, MD, MHS; and Manesh R. Patel, MD.