A nine-year collaboration between the divisions of Rheumatology and Immunology and Ophthalmology at Duke provides an uncommon, multidisciplinary approach for patients with inflammatory eye disease who present with autoimmune conditions such as uveitis, scleritis, episcleritis, or autoimmune retinopathy.
Robert T. Keenan, MD, MPH, MBA, vice chief for clinical affairs for the rheumatology division, has served as lead rheumatologist in the partnership with uvetis specialists at the Duke Eye Center. Since the creation of the clinic, patient volumes have grown steadily.
Keenan works closely with Glenn J. Jaffe, MD, an ophthalmologist and retinal surgeon in the busy clinic one day each week in the Eye Center. Three additional Duke eye specialists see patients with inflammatory eye disease within the Eye Center. A nurse practitioner with training in rheumatologic diseases works with the team.
“Rheumatologists are experiencing increases in the presentation of autoimmune diseases in general,” Keenan says. “But in this clinic, the higher volumes may be associated with a greater awareness among referring physicians and ophthalmologists that a specialized clinic exists to help with treatment of inflammatory eye diseases.”
Collaboration helps regional practices
Regional practices may not have a great deal of experience in treating eye disease with autoimmune characteristics, Keenan says. “By teaming with retinal specialists, we are able to identify and treat a wide spectrum of these inflammatory diseases, particularly the autoimmune conditions that go beyond uveitis,” he adds.
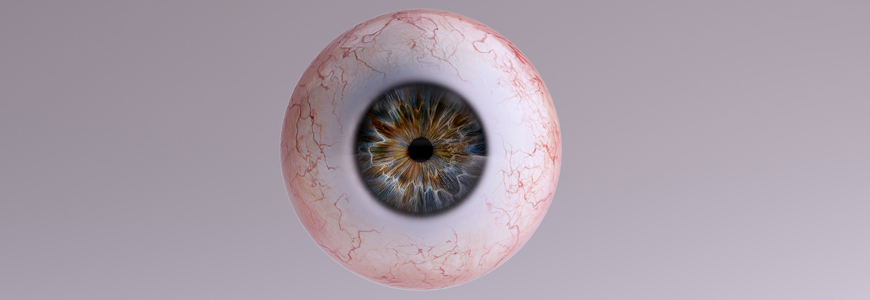
Inflammatory eye disease can affect the anterior, vitreous, and posterior chambers of the eye or all parts of the eye simultaneously. This team focuses on preventing long-term vision loss or blindness, as inflammatory eye disease is a leading cause of non-infectious, non-genetic blindness, Keenan adds.
Although inflammatory conditions present across all ages, uveitis occurs most frequently between the ages of 20 and 60, with some studies showing a higher prevalence in women with increasing age. Initial treatments are typically glucocorticoid steroids, Keenan says, but other anti-inflammatory therapies may include methotrexate, adalimumab and other immunosuppressive medications.
“Our treatment plan depends on the severity of the disease, the location, indicators of the need for a systemic approach, and any comorbid conditions the patient may have” Keenan says.