Effective patient communication following a kidney disease diagnosis is one key reason a Duke nephrologist encourages kidney specialists to consider biopsies when discussing the unexpected diagnosis of kidney failure in asymptomatic patients.
Biopsy results may help patients understand their condition as well as the course of the disease, says Duke nephrologist John V. Duronville, MD. He works closely with pathologist David N. Howell, MD, PhD, of the Duke Department of Pathology. They discuss the value and risk of biopsies as well as how they can aid patient communication.
Q: How do biopsies help patients understand their diagnosis and prepare for it?
Duronville: The nature of kidney disease is such that patients who are diagnosed with kidney disease may not understand why their kidneys are injured or failed. As a nephrologist, you have now given them what could be a terminal diagnosis, barring successful dialysis or transplant. But you have not provided an explanation of the cause of kidney damage be it temporary (acute kidney injury) or permanent (chronic kidney disease). There aren’t many other diseases or medical disciplines in which this lack of information is acceptable. Patients want to know. They have a right to know. The biopsy offers precise information that may be meaningful to the patient.
Howell: A nephrologist may learn something that is not actionable but will still help the patient understand the condition and know what to expect.
Q: At what stage in the diagnostic process is a biopsy recommended?
Duronville: The biopsy is usually the last confirmatory test. We use several blood and urine tests to find clues to the disease process affecting the kidneys. We don’t do the biopsy if we can treat the patient successfully without requesting the procedure. We make the decision to proceed with a biopsy if the cause of kidney injury remains unexplained following a thorough medical history, blood and urine analysis. We hope the results of the biopsy will give us a definitive diagnosis, help us understand the degree of damage and ultimately help us make the appropriate decisions for treatment.
Q: What are the risks associated with biopsy?
Duronville: The procedure is safe in the vast majority of cases, but complications associated with bleeding can occur. In approximately 1% of cases, we will see a post-biopsy hemorrhage. Treatment may involve blood transfusion, angiographic intervention to control bleeding or, in more complicated situations, a complete nephrectomy. We order a biopsy when we believe it will generate additional information that could change management or influence the outcome of our patient care. A biopsy can provide a diagnosis that cannot be reached with any other tactic or procedure.
Q: What kinds of diagnostic information does a biopsy provide?
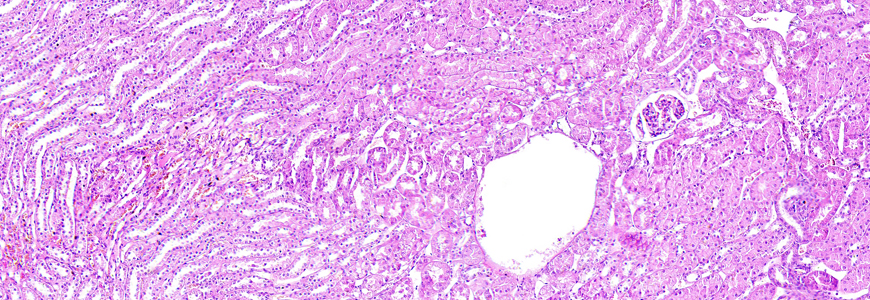
Howell: The procedure offers several diagnostic keys to the nephrologist. First and most important, what is the underlying disease? Other tests may not be effective in determining this diagnosis. Does this patient have IgA nephropathy, lupus nephritis, or focal segmental glomerulosclerosis? Second, how far has the underlying disease progressed? Often, the nephrologist has a strong impression of what condition the patient is likely to have but the biopsy provides the definitive diagnosis.
Q: How many biopsies are performed annually at Duke?
Howell: During 2018 at Duke, we performed approximately 175 native renal biopsies requested by nephrologists for a diagnostic purpose. During most 12-month periods, our pathologists interpret a total of 350 to 500 biopsies. The higher number includes those performed for native kidney diagnosis (some referred from other hospitals) as well as transplant assessment. This total does not include biopsies requested to help with cancer diagnosis.