Although awake craniotomies have been performed for years as a way to prevent harm in areas of the brain that directly control function, awake spine fusion surgery is rare, usually reserved for cases in which a patient is at risk for adverse reaction or long recovery from general anesthesia. However, because this technique typically results in quicker recovery times and requires less time in the hospital, Duke neurosurgeon Muhammad Abd-El-Barr, MD, PhD, says this approach may be applicable to a much larger segment of the patient population.
“The COVID-19 pandemic has meant that more patients don’t want to spend time in the hospital,” says Abd-El-Barr, who is one of a handful of surgeons in the United States offering this rare awake approach to spine surgery. “If patients are walking, and there are no postoperative problems, walking at home is always better than walking at the hospital.”
First Duke Patient Cases and Outcomes
The first awake spine fusion surgery at Duke was the result of a patient’s request. The patient, who was scheduled for a minimally invasive spine fusion, had had an adverse reaction to general anesthesia in the past and asked Abd-El-Barr what else was possible.
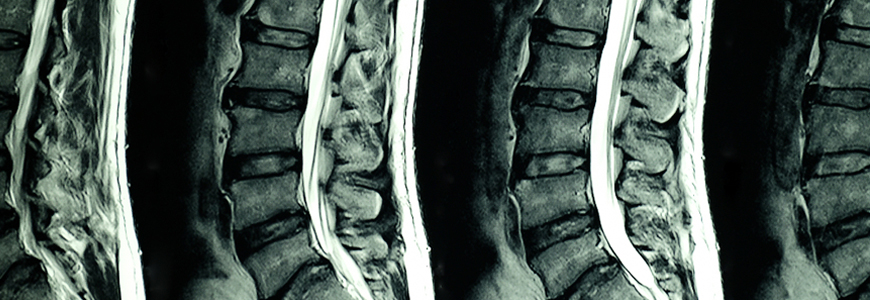
Considering the options, Abd-El-Barr performed an awake spinal anesthetic robotic lumbar fusion to treat the patient’s spondylolisthesis using a combination of decreased tissue manipulation and advanced anesthesia methods recommended by collaborators in Duke’s Department of Anesthesiology.
“In order to help accelerate and enhance the recovery for these patients, we designed an anesthetic and pain management plan that relied heavily on the use of regional anesthesia techniques, rather than general anesthesia and opioid medications,” says Jeffrey Gadsden, MD, anesthesiologist and collaborator on these cases.
Gadsden used a spinal anesthetic that numbs the patient completely from trunk to toes so that they can be comfortable during surgery with only mild sedation. Because the patient had not been completely under anesthesia during surgery, he was discharged in 24 hours.
“The patient had been in horrible pain before the surgery and had to be brought in by wheelchair, and the next day, he walked out of the post-anesthesia care unit,” Abd-El-Barr says.
After the success of the first case, Abd-El-Barr offered the new approach to a second patient, who was walking 45 minutes after surgery and left the hospital within four hours. In this case, the patient received an erector spinae plane nerve block in the pre-operative area; then, once in the operating room, spinal anesthesia was applied. This approach keeps patients comfortable for several days following the operation.
Clinical Developments and Future Work
Abd-El-Barr says several clinical developments have made this approach possible:
- Advances in minimally invasive surgery have meant there is less tissue dilation and muscle dissection.
- Advancements in long-term anesthetics allow a pain block to be placed into the muscles that releases over two days.
- Robotics allows the surgeon to place instrumentation in the spine using a robot, removing human variability and causing less trauma.
Abd-El-Barr has established a virtual awake spine study group of spine surgeons from around the world to further investigate the uses for this minimally invasive approach. One of the topics discussed by the group has been how to present the approach to patients as an option. Not all patients warm up to the idea of being awake during spine surgery, he says: “Some are extremely enthusiastic, and some say, ‘Thank you, but no.’”