Patient With Axial Myopia Sees Without Correction for the First Time
 A 44-year-old man experienced axial myopia his entire life and had never been able to see without the aid of glasses. He had an axial length of 35 mm in his right eye and 36 mm in his left, with a lens prescription of –26 diopters.
A 44-year-old man experienced axial myopia his entire life and had never been able to see without the aid of glasses. He had an axial length of 35 mm in his right eye and 36 mm in his left, with a lens prescription of –26 diopters.
When he presented to his optometrist with retinal degeneration and a retinal hole, he was referred to the Duke Eye Center. The retinal surgeon managing the retinal degeneration observed that the patient had a dense cataract in his left eye, and he referred him to Duke’s chief of Cornea and External Disease Service and director of Refractive Surgery Service, Terry Kim, MD.
Question: What new technology did Kim implement to remove the patient’s cataracts and improve his vision?
The accuracy of measurements made using ocular biometry with traditional IOL formulas—the traditional method of calculating IOL power—dramatically decreases for people with a longer or shorter eye, Kim explains. He hoped the new intraoperative aberrometry device would be better.
“We’d received the new device only about 2 weeks earlier, and I’d never used it on someone as nearsighted as him, so it was somewhat of a leap of faith,” he says. “I told him up front, 'I can’t guarantee what you’re going to be able to see without glasses or contacts.' He understood that.”
Kim was pleased to find that the new device was more accurate than traditional ocular biometry, even in a patient with a very high axial length. Although the surgery did not provide the patient with 20/20 vision, because of the retinal hole, it enabled him to pass his driver’s test without correction in his left eye in conjunction with a high-powered contact lens in his right. The procedure also allowed the patient, an avid golfer, to follow the flight of the ball, which he had never been able to do before.
“After the surgery, the patient was in tears because he could finally see something without any glasses,” Kim reports. “His parents were there and were crying tears of joy, too.”
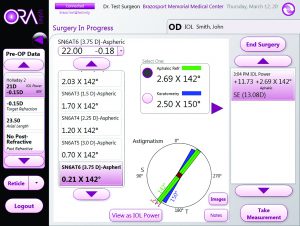 FIGURE. Representative view from the intraoperative aberrometry unit showing the preselected IOL based on preoperative biometry readings compared with the IOL choices available from intraoperative readings. IOL = intraocular lens
FIGURE. Representative view from the intraoperative aberrometry unit showing the preselected IOL based on preoperative biometry readings compared with the IOL choices available from intraoperative readings. IOL = intraocular lens
The new intraoperative aberrometry device aligns well with recent technological improvements in cataract surgery, including the femtosecond laser, he says.
“What good is it if you use a femtosecond laser to perform the cataract procedure with precision, but then you don’t have the visual result to match that accuracy?” he remarks. Had he used ocular biometry alone, he notes, the lens-power calculations would have been off by 5 to 6 diopters.
“We now have intraoperative wavefront aberrometry to give the accuracy of the lens-power selection to go along with the precision of femtosecond laser-assisted cataract surgery.”