Malcolm DeBaun, MD—a Duke orthopaedic surgeon, traumatologist, and one of the newest additions to Duke Orthopaedic Surgery—brings a focus on musculoskeletal digital innovation and the development of potentially practice-changing research applications for bone and joint health.
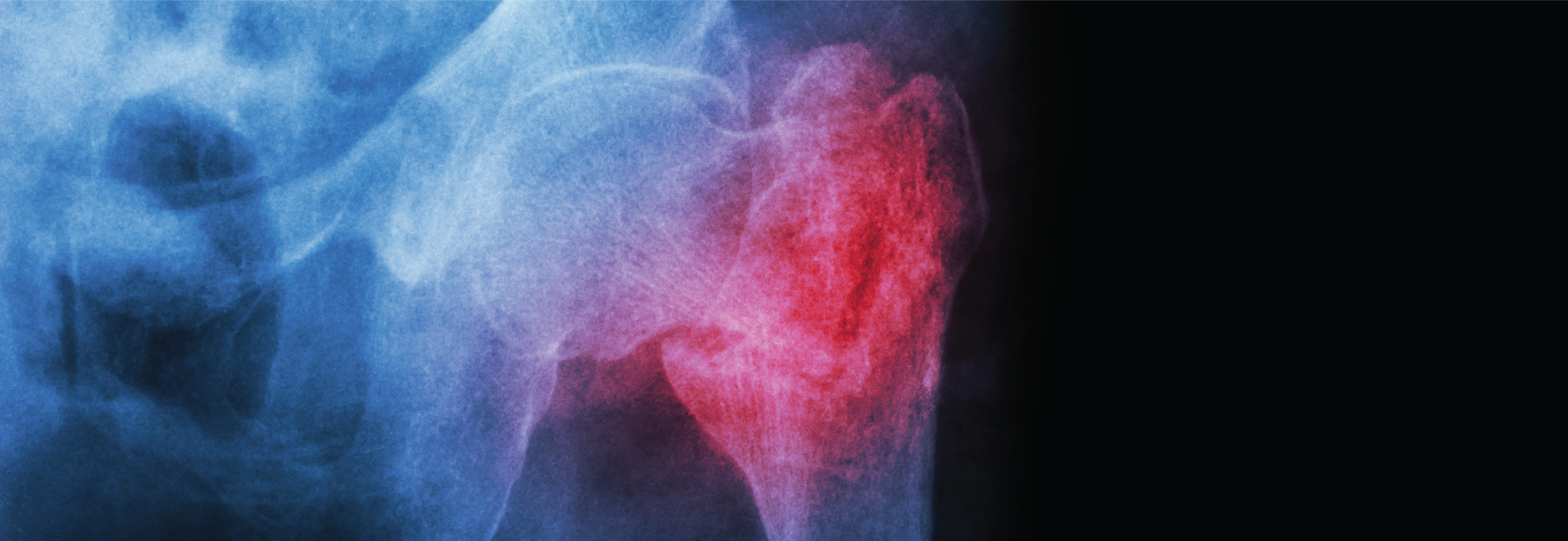
Specialized, modified instruments and implants can help facilitate high-quality restoration of anatomy after injury, he explains. One such instrument that DeBaun helped popularize based on research efforts at his prior institution is called the Black Widow, a specially engineered attachment for the Spider2 intraoperative limb positioner (Smith & Nephew, London, U.K.) that allows for adjustable distraction in cases of acetabular fracture with femoral head protrusion.
In a July 2021 JBJS Case Connector article co-authored by DeBaun, the team reports that although the use of a limb positioner had not been previously described for lower extremity procedures, it can provide appropriate on-table traction in pelvic and acetabular surgery to neutralize deforming forces and facilitate reduction and fixation.
“It's a total game-changer when it comes to reducing acetabular fractures because it can sustain traction anywhere in space for an extended period of time, and it gives you 360 degrees of control of the joint,” DeBaun says.
Another technological innovation that DeBaun helped design and patent features a new approach for performing remote patient monitoring and mobile 3-D scanning of a patient’s injury without radiographs. This technology uses a photo taken with a generic smartphone to create a 3-D diagram of the patient's surface anatomy; an artificial intelligence-assisted algorithm then analyzes the image to determine whether a fracture is present.
DeBaun’s initial publication on this developing technology, published in the April 2021 issue of Journal of Orthopaedic Trauma, explored the tool’s use in identifying and monitoring clinically relevant shoulder girdle deformity after displaced diaphyseal clavicle fracture.
“This technology will really open up a new opportunity for patients to access high-quality medical imaging—without radiation risk—that is also portable and remote,” DeBaun says. “I think this is going to revolutionize orthopaedic imaging because it makes x-rays a little less critical, and it enables orthopaedic surgeons and patients to identify bone and joint health issues without requiring an in-person visit.”
Future applications at Duke for leveraging this technology will prioritize scoliosis, DeBaun says. The team is also considering conducting new research to validate the technology for osteoporosis screening, sports medicine injury and prevention, and pediatric fracture diagnosis without radiographic assessment.
“Duke has all the resources available to further develop and use these technologies to advance patient care and really optimize outcomes,” he adds. “A surgeon who focuses on the details and has access to advanced instrumentation designed specifically to restore anatomy will benefit patients who just want to get back to their lifestyles and livelihood after sustaining an injury, no matter how big or small.”