New Treatment Paradigm for Retinoblastoma
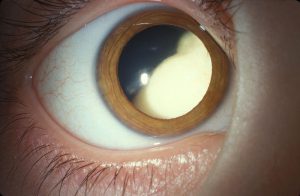
An 8-month-old infant presented to her local ophthalmologist with leukocoria and strabismus in 1 eye. Suspecting retinoblastoma, the ophthalmologist referred the patient to the Duke Eye Center, where a diagnosis of advanced somatic retinoblastoma was confirmed through eye examination under general anesthesia.
Question: What was the best, most effective treatment option for this particular patient?
Answer: The patient was treated with intra-arterial chemotherapy (IAC), an approach that allows a chemotherapeutic agent to be delivered directly into the ophthalmic artery of the affected eye via a small catheter (0.4-mm diameter). The treatment reduced the ocular tumor to one-third of its original size without any adverse effects.
Historically, enucleation or systemic chemotherapy would have been the standard treatment for retinoblastoma. However, although systemic chemotherapy spares the eye, it requires high doses, is nonspecific to the orbit, and can have severe adverse effects, including myelosuppression with risk of infection, nephrotoxicity, and hearing loss.
IAC, by contrast, allows the tumor to be selectively targeted by direct catheterization of the ophthalmic artery. This selectivity makes IAC less likely to cause systemic adverse effects, explains Miguel Materin, MD, the ocular oncologist at Duke who first saw the patient.
Although IAC is not new, it is only used at highly specialized centers because it requires the collaboration of a large, multidisciplinary team. Duke is the only place in North Carolina that offers the treatment.
For this patient, Materin worked closely with Duke pediatric oncologist Susan G. Kreissman, MD, and neurosurgeon L. Fernando Gonzalez, MD, in addition to a pediatric anesthesiologist and radiologist, among others.
“IAC is a challenging procedure that requires significant expertise from the whole team,” says Gonzalez, who specializes in vascular surgeries that require the use of small catheters to deliver treatment. “It involves directing a tiny catheter—the smallest one we have—into a tiny artery (ophthalmic artery), all in very small patients.”
During a 3-month period, the team administered 3 doses of IAC to the patient. Materin explains that, unfortunately, because of the location of the tumor—in the middle of her central vision—it is not likely that the patient will have very good vision. But, her tumor size has been dramatically reduced, and her life is no longer at risk. “The tumor looks completely regressed, and, very importantly, she will be able to keep her eye,” he reports.
“If left untreated, retinoblastoma can be very dangerous,” Materin adds. “But, with the development of better treatments like IAC, we’ve been able to reach about 95% survival in the United States.”