A new field of scientific research is examining the role that mitochondria play as a trigger of inflammation in conditions such as systemic lupus erythematous (SLE) and rheumatoid arthritis.
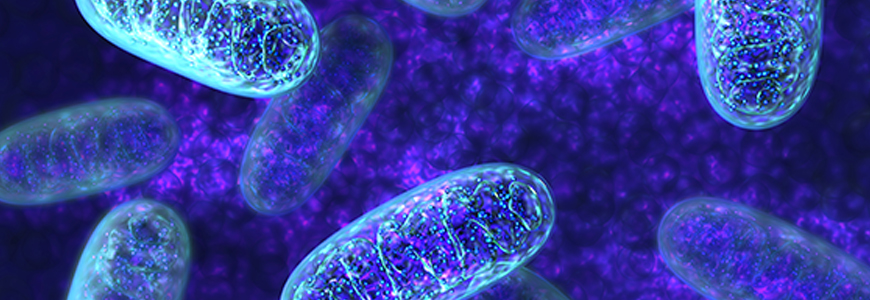
Mitochondria are intracellular organelles that have long been viewed as an essential element in metabolism, mediating the conversion of food into energy for cell development and activity. The role of mitochondria in inflammation is unexpected and the discovery of these activities offers a new perspective on the immune system.
Duke rheumatologist David S. Pisetsky, MD, PhD, a clinician and researcher, highlighted the role of these organelles in immune-mediated disease in a recent editorial in Arthritis Research & Therapy exploring the “personalities” of mitochondria.
The discoveries on the immune properties of mitochondria are based on the idea that mitochondria have developed from bacteria that have taken up residence in mammalian cells to specialize in energy generation, Pisetsky says. As descendants of bacteria, however, mitochondria have features that appear as “foreign” to the immune system and are capable of stimulating an immune response if they leave their usual “safe” intracellular location. Mitochondria even have their own DNA which resembles DNA from bacteria.
During periods of cellular stress, certain molecules can leave the mitochondria as the structures that keep mitochondria intact break down, Pisetsky writes. Once outside the mitochondria, these molecules take on new activity. A molecule called cytochrome c may interact with other molecules to drive apoptosis, a process of cell death that occurs with stress and injury. Similarly, mitochondrial DNA can interact with sensors to create inflammatory processes; these sensors are thought to respond ordinarily to DNA from viruses or bacteria that infect cells.
Role of Mitochrondia in SLE
Immunologists studying SLE, an autoimmune disease primarily affecting young women, have found that mitochondria that have escaped from cells can circulate in the blood of patients and form immune complexes with autoantibodies. In instances when whole mitochondria exit the cell, more inflammatory molecules may be released.
“This situation has led to speculation that mitochondria are important drivers of sterile inflammation and conditions such as shock,” Pisetsky suggests in the editorial.
“There’s a great deal of interest now in mitochondria, which may generally function in the same way as bacteria in cells but with significant distinctions,” Pisetsky says. “It’s become topical within the science of immunology to focus on the ways in which mitochondria promote inflammation.”
The quest to understand the role of mitochondria in immune signaling is just beginning, Pisetsky notes. Referring in the editorial to the “split personality” of mitochondria as a characterization of mitochondria’s multiple roles, Pisetsky even recommends terminology to more accurately describe the organism functions.
Highlighting the fact that mitochondria display molecular patterns that are associated with both cellular damage and infection, he suggests a more neutral term that captures the distinctive features of mitochondria: Mitochondrial-associated molecular pattern (MAMP).