Gerald A. Grant, MD, recently returned to Duke as chair of the Department of Neurosurgery after nearly 10 years with Stanford University as chief of pediatric neurosurgery, vice chair, and associate dean of faculty affairs. With technical expertise in managing childhood and young adult brain and spinal cord tumors, medically refractory epilepsy, Chiari malformations, moyamoya disease, and trauma, Grant brings a rich background of subspecialty neurosurgical care to both pediatric and adult patients in the Southeast.
In this Q&A, Grant outlines a few of his priorities for the department, new technology he plans to bring to Duke, and the translational research that his lab is leading to provide even more advanced care to patients.
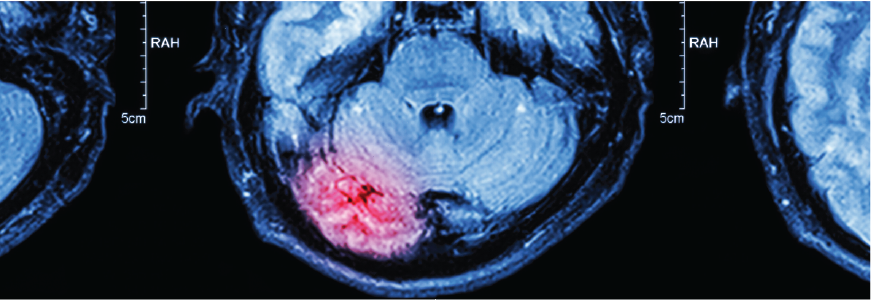
Duke neurosurgeons and brain cancer specialists offer the latest advances in medicine and neurosurgery. Our special programs focus on treating brain tumors, as well as tumors in the head and neck, epilepsy, movement disorders, cranial nerve dysfunction syndromes, peripheral nerve injuries, pain, and more.
What is one of your immediate priorities for the Department of Neurosurgery related to clinical care?
In the first few months of my tenure, I’ve been working to build a traumatic brain injury (TBI) center, which we plan to grow into a larger comprehensive center for neurorestoration following TBI. This work has included partnering with a network called TRACK-TBI, and Duke will soon become the 21st site. This renewed investment in TBI research will include developing a biobank and creating trials that will follow patients throughout their recovery process. Improving the continuity of care for TBI patients is so important, and there’s so much innovation we can bring to the table to improve quality of life in these patients.
What is your vision for neurosurgical patient care at Duke?
Neurological disorders can be really difficult to manage, and the way in which we provide our care is of utmost importance to me. I want all of our patients to feel like every person on the team has their back—we're going to advocate for them, we're going to get the best people at the table, and we're going to leave no stone unturned to help them get the answers or treatment they deserve.
What research is your team working on in your blood-brain barrier-focused lab?
My lab is highly translational to better understand how we can open the blood-brain barrier for a short period of time to deliver promising targeted agents to brain tumors. Our goal is to selectively and reversibly open up the barrier. Through our work with mice, we are able to watch fluorescent tracers cross the blood-brain barrier into the tumors in real time. We can apply these same techniques in the operating room to precisely identify the tumor margin and also to deliver catheters to the tumor bed through convection-enhanced delivery. For trauma such as TBI, we have the opposite problem: we know the blood-brain barrier opens up for a period of time after trauma, which may impede the patient’s healing process. My team is also working on ways to restore the blood-brain barrier integrity that may improve neurological function and lower a patient’s vulnerability to future concussions.
What new technologies are you planning to bring to the department?
We will soon implement a high-intensity focused ultrasound (HIFU) system, which will enable us to noninvasively treat patients with Parkinson’s or essential tremor by noninvasively ablating a very localized area deep in the brain. I am also excited about the lower frequency system which we will use as part of clinical trials to open up the blood-brain barrier to augment the delivery of agents to gliomas or metastatic tumors. We will also use this same technology to alter the electrical network in patients with epilepsy.
What do you consider Duke Neurosurgery’s advantage for patients and referring providers?
What I find extraordinary about Duke is the type and breath of cases that we’re doing, the surgical excellence and depth of experience we have here, the innovative tools that we have access to, and the respect and care we give to all patients. The collective expertise of our cranial and spinal neurosurgeons at Duke is at such a high level to manage the most complex patient conditions. Duke will soon become a destination center for several neurosurgical disorders which are best managed by a team of experts working together in collaboration.
What's also unique about Duke is that our researchers and clinicians work shoulder to shoulder to develop ideas in the laboratory at the bench, translate them in real time to the bedside, and then host those clinical trials right here at Duke to make an impact. The Preston Robert Tisch Brain Tumor Center is the best example of this collaborative approach because we have a pipeline of ideas and trials that can move quickly in a very short period of time. We are now expanding this model of innovation to other diseases such as epilepsy, movement disorders, trauma, and spine.