A Duke neurologist and neurosurgeon have collaborated to perform the first deep brain stimulation (DBS) procedures for epilepsy in North Carolina, offering a new option for patients who experience seizures that cannot be successfully managed with medical therapy.
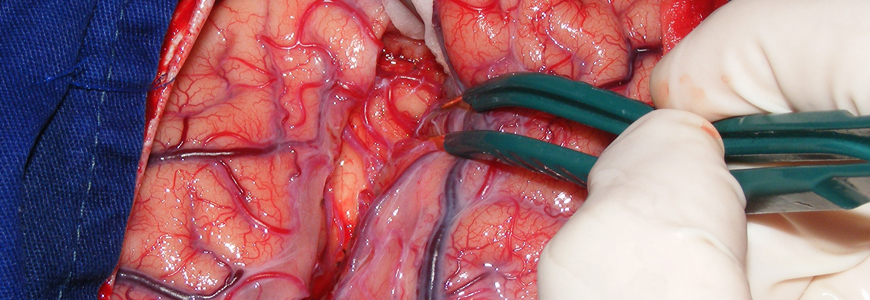
Neurologist Saurabh Sinha, MD, PhD, and neurosurgeon Derek Southwell, MD, PhD, have completed four DBS procedures in 2019 after preparing for several months to introduce the treatment option. During the surgical procedure, which is supported by real-time MRI, a DBS device is inserted into the anterior thalamic nucleus of the brain.
Though neurostimulators in other brain regions have been used for several years to treat patients with movement disorders such as Parkinson’s disease, essential tremor, and dystonia, stimulation of the anterior thalamic nucleus is a novel treatment target for epilepsy.
Specialists say thalamic DBS may offer improved therapy for epilepsy compared to other neurostimulation techniques. Vagus nerve stimulators and responsive neurostimulators, for example, reduce seizures by approximately 50-60% in patients. Sinha and Southwell say published data point to a seizure reduction of approximately 70% with DBS. In addition, the DBS may offer additional benefit in patients who already have a vagus nerve stimulator or who have undergone prior resective surgery.
Procedure will reduce seizures, decrease need for medications
“The goal of epilepsy surgery is to reduce the frequency and severity of seizures, and to help patients to decrease their requirement for seizure medications,” Southwell says. “Focal brain resection offers the best chance at seizure freedom, but it is an option only for a subset of epilepsy patients. Thalamic DBS is a new option for many of those patients, and early clinical trials show that it can significantly improve seizures and overall quality of life.”
The potential number of patients with epilepsy who could benefit is substantial, Sinha says. Many patients settle into failed medication routines after undergoing diagnosis by a general neurologist, he says, without awareness of advanced surgical options that can significantly improve quality of life.
“One of the great tragedies in epilepsy care is that we know large numbers of patients simply don’t get the care that could improve their lives,” Sinha says. “Many of these patients live with long-term, debilitating seizures and must remain on medications with complex side effects. They simply believe this is their situation. They bear it. They don’t seek additional care.”
An evaluation at a Comprehensive Epilepsy Center can help patients and families learn about diagnostic and treatment options that can have a major impact on their quality of life. DBS for epilepsy is an important addition to the options available for management of epilepsy.