Earlier intervention for children and adolescents with obesity is the key recommendation in a new clinical guideline released in January by the American Academy of Pediatrics (AAP).
Duke Children’s pediatrician Sarah C. Armstrong, MD, a longtime member and current chair of the AAP Section on Obesity, was among the physicians who developed the new guideline. Armstrong directs Duke Children’s Healthy Lifestyles Program.
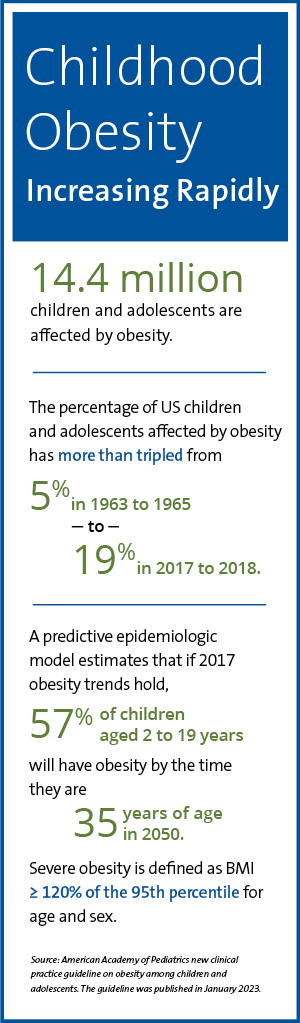
The new guideline is the APP’s inaugural recommendation for the evaluation and management of children and adolescents with obesity. Published in Pediatrics in February, the wide-ranging recommendations are framed by an emphasis on proactive, early intervention. The authors encourage physicians to consider potential contributors to excess weight in children, including social determinants of health and gaps in care for diverse patient populations.
“We can intervene in a way that is supportive and non-judgmental to help change children’s lives,” she says. “Waiting and hoping kids will grow out of their weight issue—watchful waiting—is not effective and is potentially harmful,” Armstrong says. “We have to offer a child the safest, most effective treatments available that they qualify for at that time.”
Armstrong encourages families concerned about childhood obesity to seek medical care as soon as possible and to request referral to an experienced weight-loss program with an emphasis on children and adolescents. Duke Health offers North Carolina’s only comprehensive weight loss surgery program for children under 18 years-of-age that is accredited by the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program.
In this Twitter Space, Duke faculty explore communication with children, adolescents, and their families about weight, appropriate evaluation practices, and evidence-based treatment.
Early intervention is centerpiece
Early intervention involving lifestyle modification and medication therapies is a centerpiece of the new guideline. Armstrong cautions that weight loss surgery should only be considered for patients who require an urgent intervention after other therapeutic approaches have failed.
Through a collaboration between the Duke Metabolic and Bariatric Surgery Program and the Duke Children’s Healthy Lifestyles Program, Duke Health offers the full spectrum of care, from obesity screening to surgery. “It’s rare to find all of these services in one place,” Armstrong says.
Long considered a safe, effective weight loss option for adults, studies show bariatric surgery yields better outcomes among adolescents, both in long-term BMI reduction and significant improvement or complete amelioration of comorbidities such as type 2 diabetes mellitus and hypertension, than some medical approaches.
However, the guideline emphasizes that the decision to choose surgery as a therapy for childhood obesity requires thoughtful consultation with the patient and family as well as collaboration among physicians involved in the individual’s care.
Eligibility for weight loss surgery
The new guideline defines candidates for pediatric weight loss surgery as children 13 years or older who are severely obese, falling into one of the following categories of obesity:
Class II obesity:
- BMI of at least 35
- 120% of the 95th percentile
- Diagnosed comorbid condition, such as type 2 diabetes, cardiovascular disease risks or depressed, health-impaired quality of life
Class III obesity:
- BMI of 40 or higher
- 140% of the 95th percentile
- With or without a comorbid condition
While these criteria qualify a patient for surgery, many considerations must be reviewed in determining eligibility. The AAP guideline recommends that patients be referred to a comprehensive pediatric weight loss surgery program to be evaluated by a multidisciplinary team of providers to determine the appropriate intervention.
“It’s important to note that there is not a recommendation for surgery,” Armstrong says. “The guideline recommends that providers refer patients to a comprehensive adolescent program. There’s a big difference.”
To refer a patient to the Duke Healthy Lifestyles Program, call 919-620-5356.
Benefits of referring to a comprehensive weight loss program
Physicians should consider the Duke Children’s Healthy Lifestyles Program as a referral center offering comprehensive obesity management. The program provides intensive lifestyle modification as well as targeted medications and behavioral therapy.
Patients who meet the criteria for surgery will undergo a thorough medical evaluation by a team of specialists, including a pediatrician, surgeon, dietitian, and mental health counselor. “We have case conferences during which we discuss each patient and what they need. It’s a very comprehensive and thoughtful process,” says Armstrong.
Duke weight loss surgeon Dana D. Portenier, MD, adds that a key part of this process is educating the patient. “There has to be a discussion about what the different treatment options are, understanding what the patient has tried in the past, so that you can meet them where they are,” he says. “They need to have tried other less invasive modalities first and, if those have not been successful, then they should educate themselves about bariatric surgery. We offer multiple classes and support groups to help them understand the disease process, the progression of obesity-related comorbidities, the risks of surgery and the lifestyle changes necessary to ensure success.”
