Spinal cord stimulation has proven to be a long-lasting therapy for patients with diabetic peripheral neuropathy (DPN), reducing pain, enabling greater physical activity, and improving quality of life among those whose conditions are refractory to medical management.
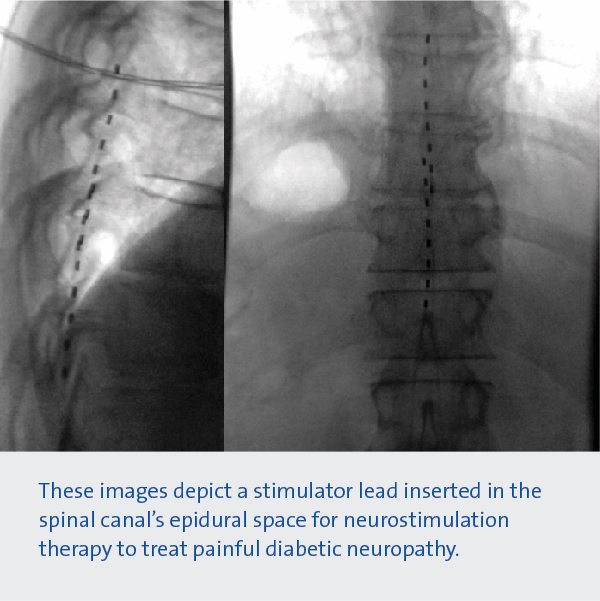
The results of a 12-month multicenter study published in Diabetes Care demonstrated the sustained effectiveness of 10-kHz spinal cord stimulation from an electrode implanted in the spinal epidural space. Due to the procedure’s relative simplicity, patients can undergo a one-week test procedure, before deciding on the permanent implantation of the device, consisting of a minimally invasive procedure consisting of a small electrode and a pacemaker.
Neurostimulation therapy, which is FDA-approved and covered by most insurance programs, is one component of a multifaceted DPN treatment strategy envisioned by Duke neurosurgeon Nandan Lad, MD, PhD, an author of the Diabetes Care study.
“What is really unique about Duke is our team approach to the treatment of DPN,” Lad says. “Not only are patients evaluated for neuromodulation therapy, but they are also seen by our endocrinology and podiatry colleagues to develop comprehensive treatment plans for each patient’s condition.”
Key points about the national trial
- Duke was one of 18 sites that participated in the trial, which enrolled patients from academic centers and community clinics. Duke specialists Susan Spratt, MD, an endocrinologist and Michael S. Kerzner, DPM, chief of the Duke Podiatry Division, collaborated with Lad.
- The study followed 216 patients who were randomly assigned to receive treatment. Six month and one-year results were reported.
- According to Lad, many DPN patients have a combination of small fiber neuropathy (burning, electric shocks, stabbing) and large fiber neuropathy (numbness, tingling, poor balance).
- Around 85% of patients were responders, with significant improvement in their DPN symptoms. The average level of pain relief was 73% and clinical trials indicate that the treatment is safe, effective, and durable.
The Duke team advocates for a programmatic approach to assist patients with DPN. Clinical management and counseling will be provided by endocrinologists, podiatrists, neurosurgeons, and neurologists as part of the comprehensive treatment program. The full scope of care encompasses diabetes education and nutrition directed by patient-centered nurse navigators.
Spratt notes that the emerging data already offers good news for patients. "Pain from neuropathy due to diabetes has traditionally been very difficult to treat,” Spratt says. “The only medical options create unwanted side effects such as sedation. This new study offers promise that patients can achieve reduction in pain as well as improvement in other factors as well.”
The case for increasing multidisciplinary care options
Around 26.8 million people in the United States have diabetes and approximately 5.3 million people with DPN. Around 2.3 million people have DPN resistant to medical management, including nerve pain medications such as Neurontin, Lyrica, or Cymbalta. "Unfortunately, current medication therapies have a low efficacy and a low rate of compliance,” said Lad.
Kerzner, whose podiatry practice serves as a primary care portal for diabetic foot conditions, says offering neurostimulation offers promising options for patients with metabolic disease complications. These patients frequently present with a variety of diabetes-related complications, including renal insufficiency, vision, and vascular problems," he explains. "We conduct a thorough evaluation of their neuropathy and are now offering neuromodulation as a new therapeutic option."
Improved neuropathy management can improve quality of life by allowing greater mobility, exercise, and stability while lowering fall risk, says Kerzner, who adds that these improvements usually extend life as well.
Although the primary objective of this study was to alleviate DPN pain, secondary outcomes included improvements in strength, sensation, and reflexes. Additionally, patients reported improved sleep, reduced pain interference, and improved functioning. The Duke team stated that it was remarkable how there was an improvement in so many areas and that this represents the first truly neurorestorative treatment for DPN. They concluded, “We are excited to offer this therapy as part of the Duke Program for Diabetic Peripheral Neuropathy's comprehensive team approach."