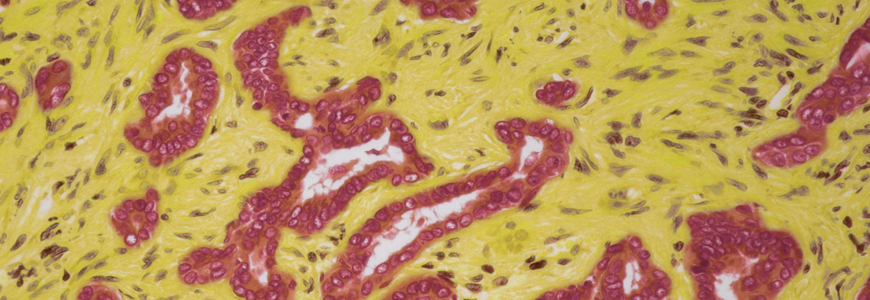
A 34-year-old woman presented to Duke with primary sclerosing cholangitis (PSC) and ulcerative colitis, affecting her immune system, liver, gallbladder, and bowel. An imaging study also showed some abnormalities in her bile ducts. Under the care of hepatologist Carl L. Berg, MD, she underwent endoscopic retrograde cholangiopancreatography, which revealed cholangiocarcinoma, a rare form of cancer that begins in the bile ducts.
“One of the dreaded complications of PSC is the development of cholangiocarcinoma. There are no great guidelines for how to detect it in people with PSC, and it’s a terrible event, particularly if you don’t catch it early enough,” Berg says.
Question: What curative therapy did Berg use to treat the cholangiocarcinoma?
Answer: Berg coordinated with colleagues in interventional endoscopy, radiation oncology, and medical oncology to create a treatment protocol that would downstage the tumor while the patient awaited liver transplantation. After six weeks of radiation therapy, the patient was given chemosensitization via capecitabine and then stayed on chemotherapy until transplantation, which was performed within six months of diagnosis. (Because cholangiocarcinoma is considered lethal, patients with this disease receive extra priority in the national United Network for Organ Sharing system, with a high Model for End-Stage Liver Disease score.)
Prior to this patient’s transplantation, the multidisciplinary team worked together to rigorously confirm through a series of endoscopic ultrasounds and lymph node biopsies that no cancer had progressed beyond the woman’s liver. Surgeons also confirmed there was no evidence of spread within the abdomen at the time of transplantation.
“If you do the transplant and there are cancerous cells that have escaped the liver, the survival rate is usually less than a year, as the malignancy tends to spread quite rapidly under immunosuppressants,” he explains.
Although chemotherapy and radiation therapy do not cure cholangiocarcinoma, they have been shown to markedly reduce risk of recurrence; however, they also make the surgery more technically difficult, causing especially fragile blood vessels and localized scarring that surgeons must work around during the operation. “Many centers do not perform transplants for patients with cholangiocarcinoma because it’s complicated and takes a real team to successfully get these individuals to transplantation with a good long-term survival with a scarce resource like livers,” Berg says.
As medical director of abdominal transplantation at Duke, Berg, in conjunction with abdominal transplant surgeon Stuart J. Knechtle, MD, radiation oncologist Brian G. Czito, MD, and medical oncologist Michael A. Morse, MD, MHS, led the creation of Duke’s multidisciplinary protocol to enable patients with cholangiocarcinoma to successfully come to transplantation, combining information from the literature and their own experiences.
Berg credits Duke’s success in transplantation to this multidisciplinary approach and a shared philosophy toward patient care. “Duke has the geographically and philosophically localized expertise to do very complicated things in transplantation,” he says. “We are fortunate to have great partnerships with people that surround us in the transplant arena where we work directly and in a concerted manner with specialists who have an interest in caring for our complicated transplant population.”
In the four years since transplantation, the patient has had no evidence of recurrence, and her liver function is normal. Despite some additional complications from her existing ulcerative colitis that required the removal of her colon, she even delivered a healthy baby in April 2019 while continuing to receive care from Berg and specialists in the Maternal-Fetal Medicine Division of Duke’s Department of Obstetrics and Gynecology.
Duke’s transplant program has one of the best one-year patient survival rates out of 147 transplant programs in the United States, according to data from the Scientific Registry of Transplant Participants. Berg attributes this success to the systemized multidisciplinary interactions: “A major theme for our success is that our offices are in the same place, we share clinic space every single day, and we have regular meetings with our oncology colleagues to discuss and manage these complex cases.”