Though endoscopic neurosurgery is not yet common around the world, Patrick Codd, MD, a Duke neurosurgeon, says many patients ask specifically about keyhole brain surgery, a minimally invasive way to perform cranial surgery and improve postoperative healing time.
“With advances in neuroanesthesia and other medical technology, many of the larger surgeries that are still most common across the country are no longer necessary if these novel techniques are used,” Codd explains. “Because those old styles of surgery require disruption of large portions of scalp and skin as well as removal of large portions of skull, they put patients at higher risk for infection, cause more pain, and require a longer recovery times.”
Alternatively, a keyhole surgery often requires as little as a 1- to 2-inch diameter entry that enables the surgeon to operate only on the area of the brain they need to access. “The less tissue that needs to disrupted and the less amount of brain exposed to the outside world, the better it is for the patient and their healing,” Codd adds.
Though this approach is not a one-size-fits-all surgery, Codd says that by using smaller instruments, computer navigation, and high-resolution imaging systems, “we can build a customized approach for the patient’s individual and unique situation, which allows us to safely do the same surgery with much less risk.”
Advances in Minimally Invasive Brain Surgery at Duke
To support this newer treatment option, researchers in Duke's Brain Tool Laboratory—a collaborative engineering endeavor that Codd manages—have developed technologies to improve the delivery of minimally disruptive care to patients.
“At Duke, we're trying to unite the high-technology frontier surgery with a more humanized patient care experience,” Codd explains. “A person doesn’t care what kind of computer I roll into the OR; they’re looking for someone who can help them get through what’s happening in their brain. We want patients to know that they’re coming into a customized care experience that is a much more intimate clinical encounter about their issue.”
Latest Developments from the Brain Tool Laboratory
The latest developments from the Brain Tool Laboratory include the following:
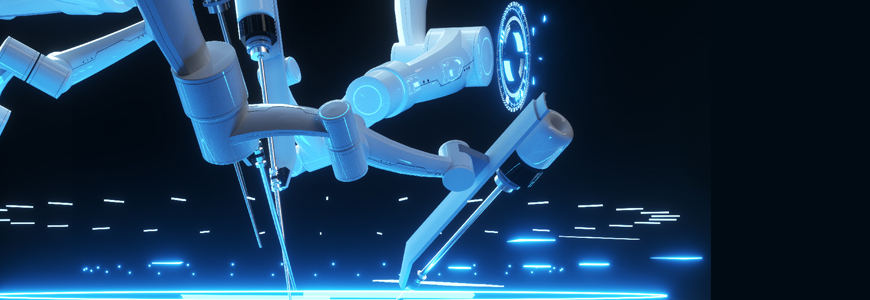
A robotic platform that automatically targets and eliminates tumor tissue down to much higher precision than a human surgeon. This system integrates high-resolution imaging, computer vision, optics, and lasers to precisely target and eliminate the tumor tissue. The technology is still exclusively being tested in the lab, Codd says, but the team hopes it will ultimately provide a tool capable of performing these delicate tumor resections with precision, safety and effectiveness unmatched by today’s surgical standards.
“With the complexity of the imaging systems we have and the resolution we can achieve with our current technologies, there will come a time when mechanical manipulation is not going to be as precise, safe, or accurate as what we can achieve with a system like this that integrates all this information and assist surgeons,” he adds.
A brain tumor identification system. This OR system casts a blue light on the surface of the brain and uses machine learning algorithms to distinguish tumor from normal brain tissue.
“This technology alone has applications in the OR for helping surgeons figure out when they’re operating where the boundary of the tumor is, as it’s very subjective as we look at consistency, feel, and color of the tumor as current guides to what is tumor and what is not,” Codd notes.
Future studies, slated to begin in the next few months, will analyze the percentage of chance that tissue identified is tumor, which would help maximize resection while minimizing potential for injury surrounding normal brain tissue, he adds.
Surgical instrument tracking system. Using radio-frequency identification on instruments supplied for use in the OR, this system has helped increase efficiency and cost savings by tracking instruments actually used during a typical procedure.
“For instance, when I’m doing craniotomy for a tumor, I used to get 150 instruments, but only used 35,” Codd explains. “Every one of those unused instruments has to be packaged, washes, counted, and packed back up, which is wasteful.”
This system helped Duke University Hospital to reduce the number of surgical instruments in his craniotomy by tray by about 70%, Codd says, and is being expanded for use across the health system.
“The tracking also enables us to predict the timing of use of an instrument, what might be coming next, and when and how the timing of surgery might work,” he adds. This improved efficiency translates to a smoother experience for the patient and their care team, while reducing waste and making the operating room smarter.