Managing, Mitigating Risk With a Rare Familial Syndrome
After learning that a family member had been diagnosed with medullary thyroid cancer and was a carrier of the rare, familial cancer syndrome multiple endocrine neoplasia type 2A (MEN 2A), a 64-year-old former Pennsylvania police officer underwent testing to determine if he also harbored the dominant mutation.
Despite being asymptomatic, he also was confirmed to be a carrier of MEN 2A, which increased his risk of developing multiple endocrine tumors, including a rare form of thyroid cancer.
After researching centers that specialize in treating patients who are carriers of MEN 2A, the patient chose to pursue further evaluation and treatment at Duke and was referred to endocrine surgeon Sanziana Roman, MD. The patient expressed that he wanted to avoid surgery, if possible.
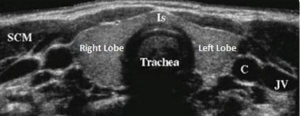
Roman performed ultrasonography of the patient’s thyroid, the results of which did not reveal cancerous nodules. Laboratory testing also showed that his calcitonin levels were low—a finding that was reassuring.
Question: Knowing the risks associated with being a carrier of MEN 2A, what did Roman recommend to manage the patient’s health now and in the future?
Answer: Given the patient’s age, Roman recommended preventive thyroidectomy to remove any undetected, early-stage cancer and prevent thyroid cancer from developing later in life.
“Even though tests did not detect the clear presence of cancer, given that he was an adult, I was concerned,” says Roman. “The only way to know for sure is to remove the thyroid. I had to convince him it was the right thing to do.”
Generally, if an adult patient is identified as a MEN 2A carrier, the recommendation is thyroidectomy, Roman explains. When MEN 2A is identified in children, a recommendation is made based on the specific genetic mutation and the age of the child, which can determine when the thyroid should be removed to prevent thyroid cancer from developing in the future.
After conducting tests to rule out the presence of an adrenal tumor (another possible MEN 2A–associated tumor), Roman performed thyroidectomy and discovered very early-stage cancer in the patient’s thyroid.
“Sure enough, the patient had microscopic areas of cancer,” says Roman. “Because we caught it very early, we are able to prevent it from advancing and metastasizing.”
Following thyroidectomy, the patient did well and continues to be monitored by his local endocrinologist to manage his hormonal levels and any related issues. He will also return to Duke once a year to rule out recurrence and other endocrine tumors, such as pheochromocytoma. His follow-up care will be life-long.
“If a patient carries the RET mutation, there’s a close to 100% chance of him developing medullary thyroid cancer,” says Roman. “The only way to prevent it is to remove the thyroid. The longer the patient waits, the higher the risk of developing cancer. This cancer is different in that, even when caught early, it could metastasize.”
Roman continues: “This patient did his own research, chose to be treated at a center with experience with the mutation, and had a good outcome. At Duke, we are well-equipped to work remotely with patients’ local doctors and ensure there’s a multidisciplinary team providing excellent, seamless care.”