Despite being born after a normal pregnancy and delivery, a newborn baby girl was immediately noted by medical staff to have extensive nevus flammeus covering large areas of her body. Commonly known as port-wine birthmarks, the condition is characteristic of the rare disorder Sturge-Weber Syndrome (SWS), which is often associated with seizures and glaucoma.
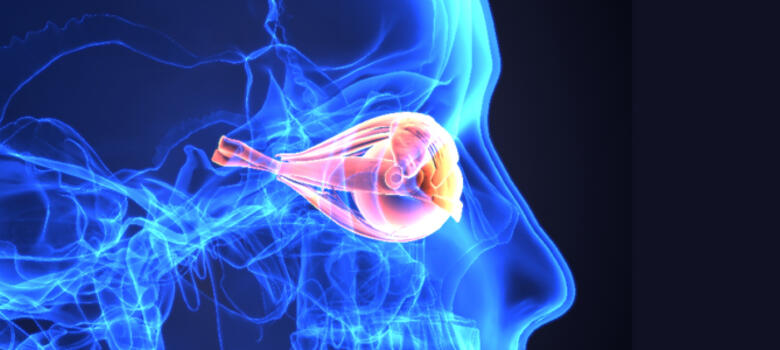
A number of other potential abnormalities were also quickly detected, but a full-body MRI and ultrasound failed to confirm any obvious abnormalities other than the widespread port-wine birthmarks, including in the V1 distribution on the left side of the baby’s face. The baby’s parents quickly became health care advocates for their child, and ophthalmologists eventually confirmed she had several ongoing issues in her left eye, including ocular hypertension, mild haziness of the cornea, and possible accelerated eye growth. The issue of whether this was truly glaucoma was somewhat less clear, as was the decision regarding whether and how to treat the left eye.
Several of the nation’s leading pediatric ophthalmologists recommended the child’s parents seek insight and treatment from Duke Eye Center’s Sharon Freedman, MD, professor of ophthalmology and pediatrics division chief, who is a world-renowned expert and foremost authority on childhood glaucoma. The patient’s father, himself a physician and surgeon, contacted Freedman and provided detailed information from visits and examination under anesthesia with two prior well-known ophthalmologists, as well as data from his own measurements of his daughter’s eye pressures at home while she was sleeping. He expressed the difficulty of not knowing whether his daughter simply had ocular hypertension (elevated eye pressure without structural or vision damage to the eye) or actual glaucoma (damage to the eye from the elevated pressures); hence, the challenge of whether and how to treat her affected eye.
“We did an initial telehealth visit to discuss the past data the doctors and the father had collected and options for how I felt one could proceed going forward,” says Freedman. “It was challenging to obtain eye pressures in the child because she did not cooperate with testing in the office (or at home) when she was awake.”
The baby’s father purchased an iCare rebound tonometer (iCare, Helsinki, Finland) so that he could obtain valuable intraocular pressure (IOP) measurements to guide treatment decisions without the need for the child to undergo so many examinations under anesthesia, especially those simply for IOP monitoring. He also purchased a handheld camera to image his daughter’s optic nerve over time to help determine its current health and whether it was changing over time.
“In-home eye pressure monitoring can provide invaluable information to the treating physician and the patient’s family, in cases of known or suspected glaucoma, especially when it provides real-time pressure values at different times outside of normal office hours,” Freedman explains.
Although not yet widespread in its implementation, Freedman believes home IOP monitoring will increase in prevalence in the future and has developed a lending library for home tonometry devices. Selected patients are given the devices for home monitoring of IOP over a period of weeks or months to optimize management of childhood glaucoma.
The family traveled to Duke Eye Center in September 2020. Freedman performed spectral domain optical coherence tomography (OCT) imaging of the child’s optic nerves, maculae, and the choroidal hemangioma in the affected left eye. “This imaging, allowing a quantitative optic nerve head health assessment, was possible only through an ongoing research study at Duke because the device which holds the OCT horizontal (rather than vertical for tabletop imaging) to allow imaging of a supine patient is not yet FDA-approved,” says Freedman.
OCT imaging suggested that there was a slightly thinner peripapillary retinal nerve fiber layer thickness in the affected right vs. the normal fellow eye, making the likely diagnosis mild glaucoma rather than ocular hypertension, and Freedman performed goniotomy surgery. “This so-called ‘angle surgery,’ which is very low risk and takes only a few minutes to perform, is a microsurgical technique that allows the surgeon to cut through the inner portion of the trabecular meshwork for about 80% of the circumference of the entire eye, thereby allowing aqueous humor to bypass that tissue and flow directly into the canal of Schlemm,” Freedman explains.
The patient tolerated the procedure well, and three months later, the 1-year-old child recorded an album of songs with her older sister.
“We’re now monitoring her optic nerve carefully while she continues to be treated with eye drops to lower the pressure as much as much as possible,” Freedman says. Follow-up imaging in subsequent examinations will either confirm stability or show progression of pressure-related changes to the left optic nerve, which would necessitate additional pressure-lowering intervention.
“Episcleral venous pressure is often elevated in eyes with SWS-associated glaucoma, and there is no specific treatment for that condition at this time,” says Freedman. Duke Eye Center will soon be a test site for an experimental drug designed to specifically lower episcleral venous pressure. Adult patients with SWS-related glaucoma or elevated eye pressures will be the first to receive the treatment.