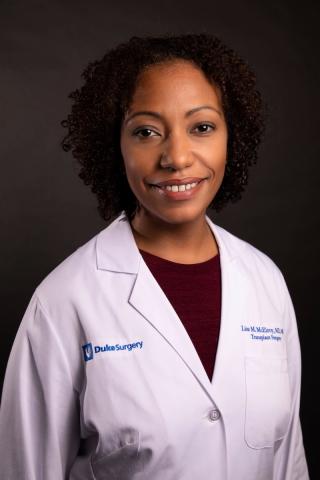
An effort to increase access to organ transplant for historically marginalized populations has been launched by a team of Duke surgeons and specialists led by Lisa McElroy, MD, MS, an abdominal surgeon and researcher.
An essential component of equitable access to transplant is a uniform, transparent process of assessing patients for addition to the waitlist, McElroy says. The evaluation process varies among clinicians and centers, she adds, emphasizing the need for better data architecture and risk assessment tools.
“Several different clinicians assess specific aspects of candidacy when evaluating patients,” McElroy says. “Then we come together as a selection committee to make a final decision about who gets added to the waitlist. Patients’ individual challenges and the complexity of the process have led to lower rates of waitlist additions for marginalized populations such as women, racial and ethnic minorities, and patients with low income or education levels,” she explains.
In addition to McElroy, team members are William Knechtle, MBA, MHA, innovation program manager for the Duke Institute of Health Innovation (DIHI), Connor Davis, MS, of the Duke Big Ideas Lab, and Mark Sendak, MD, MPP, DIHI clinical data scientist, Wendy Webster, MBA, and Hamed Zaribafzadeh, PhD, from the Department of Surgery’s Laboratory for Transformative Administration.
Duke physician team members serve as liaisons to the transplant center referral community and clinical operations. They include Stuart J. Knechtle, MD, the executive director of the Duke Transplant Center, Debra L. Sudan, MD, chief of the Abdominal Transplant Surgery program, Scott L. Sanoff, MD, a transplant nephrologist, and Julius M. Wilder, MD, PhD, a gastroenterologist and hepatologist.
New mechanisms for tracking patients through the transplant process
The team is creating a mechanism for tracking patients through the transplant selection process and developing a digital innovation that displays key patient data in a consistent format to support efficient and equitable assessment for the waitlist. Simultaneously, an effort is underway to develop a patient-facing tool, such as Duke MyChart, to keep patients informed and engaged.
“My interest is in improving access to organ transplant for populations that are historically marginalized,” says Dr. McElroy. These populations include racial and ethnic minorities, women, and people who are uninsured, unemployed, or lack financial resources.
The project is one of 10 high-potential initiatives supported with funding in 2021 from DIHI. The grants promote novel strategies to improve health care delivery, increase equity, promote digital solutions, and improve provider and staff experiences.
The effort aims to address the difficulties faced by marginalized populations in completing the rigorous transplant assessment and being included on a waitlist. “DIHI has been a wonderful partner in this work. They are invested in innovative projects that address major health challenges and are used to tackling complex problems in the clinical enterprise,” McElroy says.
“Dr. McElroy’s research and pragmatic implementation efforts will have transformational effect in developing awareness and support the building of equitable clinical programs in transplant,” says Suresh Balu, MS, MBA, DIHI program director and associate dean for innovation and partnership for the Duke School of Medicine.