Duke Raleigh Hospital’s Head and Neck Oncology program has begun offering specialized care for patients at risk for developing advanced skin cancers following an organ transplant.
Patients who have undergone transplantation—particularly a solid organ transplant—are at high risk for developing skin cancer due to their immunosuppressed state, explains Trinitia Y. Cannon, MD, a Duke head and neck and microvascular surgeon. She leads a multidisciplinary head and neck oncology clinic in Raleigh, with clinicians who specialize in diagnosing and treating growths, tumors, and cancers in the head and neck region.
“When thinking about referring a patient with skin cancer, a lot of providers think to refer only to Dermatology. However, patients with advanced skin cancers that are close to or involve the lips, eyes, scalp, ear, or ear canal will require a multidisciplinary approach,” Cannon says.
Cannon leads these complex head and neck surgeries in Wake County and works together with several other Duke teams to coordinate and navigate the care for this patient population. In addition to Cannon, specialized team members include neuro-otologists, neurosurgeons, transplant specialists, dermatologists, and medical and/or radiation oncologists.
“We work closely with our Dermatology colleagues, but our team is available to see those patients who will require a more extensive resection, one that involves removing the parotid gland, the eye, or nose, as these patients are more likely to require advanced reconstruction,” adds Cannon.
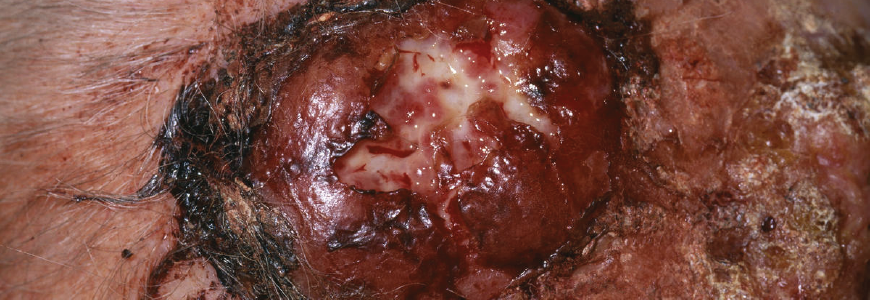
High-Risk Skin Cancer Presentation and Treatment
Patients may initially present with a small skin cancer involving the face but later develop a facial nerve paralysis or a lymph node/mass in the parotid or neck. Additionally, patients may get referred directly to the radiation and/or chemotherapy team because they present with a neck mass, unaware that it may be related to skin cancer.
“Oftentimes, we see these patients at the point when their condition is too advanced for us to treat because the mass has been treated as a lymph node, virus, or upper respiratory infection for some time, because the connection isn’t always clear between the two presentations,” Cannon says. “But if a patient has a mass on the same side that they had a cancer that was removed, even if it was a few months earlier, it should be considered cancer until proven otherwise.”
The surgical approach most commonly used to reconstruct these extensive high-risk skin cancer cases usually involves a free flap surgery, a technical procedure that involves removing tissue from the forearm, thigh, fibula, or scapula and transferring it to a new location to rebuild soft tissue and/or bone that was removed during the cancer resection. Smaller cases may need a different type of rotational flap that will cover the affected area of the head or neck.
For an advanced skin cancer involving the ear canal, the team-based procedure flows as follows:
- The head and neck surgeon (neuro-otologist) drills out the patient’s mastoid bone in the back of the ear. Depending on the tumor location, this may require a neurosurgeon to resect the dural lining of the brain.
- The head and neck surgical oncologist then resects the skin, ear, and facial nerve from the patient’s parotid gland and cleans out the lymph nodes in the neck.
- A neuro-otologist then resects the bony portion of the ear canal in order to remove the tumor in one block and cleans out the bone and back of the ear.
- Once the neurosurgeon checks for any brain fluid leaks and repairs any defects, the reconstructive surgeon then completes the surgery using a free flap.
- Patients are often recommended for radiation and chemotherapy afterwards to ensure the cancer is eradicated.
Refer a Patient
“We work collaboratively with teams in the community, and we’re here to be a partner in your patient’s care journey,” Cannon says.
To refer a patient, log in to Duke MedLink or call 919-485-1900.