Sentinel lymph node (SLN) mapping has gained acceptance in recent years as an effective technique for the surgical staging of uterine and cervical malignancies. However, the dye most commonly used for mapping—isosulfan blue—fails to identify bilateral SLNs in as many as one-half of patients. As a result, per many well-accepted algorithms, these patients often undergo complete pelvic lymphadenectomy, which is associated with increased surgical time and risk.
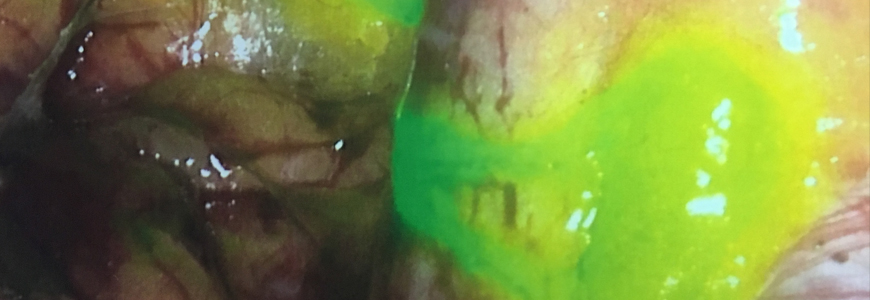
In a new prospective, multisite study published in August 2018 in Lancet Oncology, investigators found that indocyanine green dye is superior to isosulfan blue for identification of bilateral SLNs in patients with clinical stage 1 uterine or cervical cancer. The findings suggest that adoption of indocyanine green dye as the standard of care will improve surgeons’ ability to make treatment decisions and reduce surgical morbidity.
“To be accurate, given the study was designed as a noninferiority trial, we cannot technically state superiority,” notes study co-author Paula Lee, MD, MPH, a gynecologic oncologist at Duke. “Having said that, the results clearly showed that indocyanine green dye had significantly higher SLN detection and bilateral mapping rates.”
In the phase 3 Fluorescence Imaging for Lymphatic Mapping (FILM) trial, 180 women with clinical stage 1 cervical or uterine cancer at eight sites were randomized to undergo lymph node mapping with either isosulfan blue dye followed by mapping with indocynanine green and near-infrared imaging or the reverse. Once mapping was complete, LNs identified with either dye were resected.
Although the trial was designed as a noninferiority study, researchers found that indocyanine green dye was significantly superior to isosulfan blue. Of the confirmed lymph nodes excised (485), 97 percent (471) were identified with green dye, whereas only 47 percent (226) were identified with blue dye. Bilateral SLNs were identified using indocyanine green in 82 percent of patients versus 32 percent of patients using isosulfan blue dye.
In a post-hoc analysis, the researchers also found that, unlike isosulfan blue, the indocyanine green dye successfully identified all metastatic SLNs. No adverse events were associated with either dye.
Some previous studies have suggested that indocyanine green is safe and feasible and potentially superior to isosulfan blue for lymphatic mapping in solid tumors. However, these studies were small and retrospective, and the application of indocyanine green dye for lymphatic mapping has been limited to off-label use.
The FILM study is the first prospective, randomized controlled trial to compare the use of indocyanine green dye with the current standard of care for lymphatic mapping. Based on the results, the indocyanine green dye manufacturer submitted an application to the FDA for the on-label use of indocyanine green combined with near-infrared imaging for lymphatic mapping.
“The results of this study will hopefully define the standard of care surgical technique for SLN mapping in clinical stage 1 uterine or cervical cancer,” Lee concludes.